How Come They're Happy and I'm Not? (16 page)
Read How Come They're Happy and I'm Not? Online
Authors: Peter Bongiorno

Tryptophan can be found in all protein foods in small amounts. Relatively high amounts are present in bananas, turkey (which may contribute to the Thanksgiving sleepiness many people experience), red meat, dairy products, nuts, seeds, soy, tuna, and shellfish. There are no food sources of 5-HTP.
Catecholamines refer to the two neurotransmitters epinephrine and norepinephrine (called adrenaline and noradrenaline in England). These are made by your adrenal gland and help you feel awake, alert, and motivated. Major symptoms of depression can arise from catecholamine deficiency.
As tryptophan and 5-HTP are to serotonin production, L-phenylalanine and tyrosine are to the conversion to first dopamine (DA) and then onto epinephrine and norepinephrine (NE).
The Phenylalanine Tyrosine Neurotransmitter Pathway
Phenylalanine → PEA → Tyrosine → Dopamine → Epinephrine
and Norepinephrine → Better Mood
CLINICAL CASE: LENORE AND 5-HTP
One very depressed and anxious forty-eight-year-old patient, “Lenore,” visited my office after she had tried five different antidepressant drugs over a three-year period. After listening carefully to her story and asking for some testing, I learned her thyroid function was suboptimal; her vitamin D, B
12
, and iron were low; and her early life experiences produced negative thought patterns that did not allow her have a more positive outlook.
To help, I prescribed for Lenore some essential fatty acids, vitamin D, B
12
, and iron as well as thyroid support. We worked on her digestion in order to allow better nutrient absorption. I also prescribed 100 mg of 5-HTP twice a day and recommended acupuncture. Meanwhile, she started to work on her negative thought patterns. Her depression lifted in about one month after starting treatment, and she no longer required antidepressant medication. While no medication had seemed to help, an approach working on multiple levels of her health at the same time did the trick.
Phenylalanine is a precursor of brain phenylethylamine (PEA), an amino acid derivative that contributes to overall energy and elevation of mood. Phenylalanine converts to tyrosine, which is in turn converted to dopamine, and subsequently norepinephrine and epinephrine, which stimulates the nervous system. Studies of people who were both phenylalanine and tyrosine depleted paint a picture of those who are less content and more apathetic—does this describe how you feel sometimes?
There are few good depression studies of phenylalanine or tyrosine. In 1975, twenty-three depressed people who didn't respond to drugs were given 50 or 100 mg per day of phenylalanine for fifteen days. By the thirteenth day of treatment, seventeen subjects reported normal mood. A second study in 1986 showed that phenylalanine supplementation elevated mood in thirty-one of forty depressives with 14 g doses of phenylalanine.
Tyrosine may help your body deal with stress and difficult challenges. It significantly helped the symptoms, adverse moods, and performance problems in subjects exposed to 4.5 hours of excess cold and lack of oxygen in a 1989 study. Tyrosine has also been shown to significantly improve mental performance in those with sleep deprivation.
If you are overweight, have a strong appetite, experience regular pain (maybe migraines or arthritis), are going through a lot of physical stressors, or have low motivation and apathy, these amino acids may be able to help. I have used tyrosine and glucose tolerance factor (GTF—a supplement that is composed of a natural form of chromium) to help lessen tobacco withdrawal symptoms in patients who were trying to quit smoking.
The L form of phenylalanine may be dosed up to 14 g a day in divided doses. The D form of phenylalanine has been studied in doses of 350 mg per day. As an antidepressant strategy, L-tyrosine may be used in 500 to 1,000 mg doses two or three times a day, with some studies dosing up to 6,000 mg per day in total. Because tyrosine can be stimulating, taking it during the daytime and adding 1,000 to 1,500 mg of L-tryptophan or 50 to 100 mg of 5-HTP at night for sleep may be a good therapeutic combination to help in mild to moderate depression. No known studies have used phenylalanine and tyrosine at the same time.
Taking too much of these amino acids for your body may result in increased blood pressure and emotional jitters, trouble
sleeping, or headaches. Phenylketonuria (PKU) is a disorder in which the body fails to turn phenylalanine into tyrosine properly. Those with PKU should not supplement with phenylalanine and should also be wary of artificial sweeteners, which sometimes use it. Have you ever noticed the warnings on diet soda labels?
Tyrosine seems to be generally safe, though doses greater than 9 g have yielded reports of nausea, diarrhea, headache, vomiting, or excessive nervousness. Insomnia can be prevented by avoiding evening supplementation. Tyrosine should not be taken by anyone who is taking monoamine oxidase inhibitors (MAOIs) for depression or by patients with high blood pressure. Tyrosine may also be contraindicated in multiple myeloma, a cancer of bone marrow cells. Patients with Graves' disease or an overactive thyroid should use caution when supplementing with tyrosine because it might boost thyroid hormone levels.
Some of the most concentrated sources of phenylalanine are torula yeast, soybean protein isolate and concentrate, peanut flour, dried spirulina, seaweed, defatted or low-fat soy flour, dried and salted cod, dried or frozen tofu, Parmesan cheese, almond meal, dry roasted soybean nuts, dried watermelon seeds, and fenugreek seeds. Tyrosine is found in fish, soy products, chicken, almonds, avocados, bananas, dairy products, lima beans, and sesame seeds.
Along with your fatty acids, phosphatidylserine is a major component of your brain nerve cell membranes. It plays a crucial role in the modulation of the stress hormone cortisol, which is known to remain at high levels in depressed people and can destroy areas of the brain when it sustains at high levels. Phosphatidylserine can help reduce your level of cortisol and protect your brain.
In two studies, 800 mg per day of phosphatidylserine followed by exercise lowered cortisol. A study of ten elderly women with
major depressive disorders, found that 200 mg daily improved depressive symptoms and memory.
I typically recommend phosphatidylserine for people dealing with great physical stress, poor memory, and high cortisol. You can ask your naturopathic doctor or other holistic practitioner for a saliva cortisol test if you would like to check levels of cortisol in your system. You can take 200 to 800 mg of phosphatidylserine in divided doses per day on an empty stomach. It may be especially useful before stressful situations. One study of 130 patients showed no negative side effects—it was actually a benefit to liver function.
The sources with the highest levels phosphatidylserine are mackerel, herring, chicken liver, tuna, soft-shelled clams, and white beans. With the exception of the white beans, vegetables overall have insignificant quantities.
S-adenyosyl-L-methionine (SAMe) is a naturally occurring molecule involved in the synthesis of various neurotransmitters in the brain. SAMe is not new—its chemistry was described in 1952. It has been in use for decades in Europe and is a prescription medication in Italy, Spain, Germany, and Russia.
Although the antidepressant mechanism of SAMe is not fully clear, with folic acid and B
12
, it helps create neurotransmitters such as dopamine, serotonin, and norepinephrine—all of which are needed for good mood.
Folate-B
12
/SAMe Pathway
Folic Acid + Homocysteine + B
12
(Methylation Reaction) →
Methionine → SAMe → Dopamine/Serotonin/Norepinephrine →
Good Mood
Without enough SAMe, your body cannot build well-formed fatty myelin sheaths for your nerve cells, which are needed for healthy nerve cell electrical conduction. Low SAMe is associated with high homocysteine levels (see
chapter 4
), which can increase the brain toxin glutamate. Homocysteine also breaks down the linings of vessel walls, contributing to inflammation and heart disease. All these promote the development of various disorders, including depression, and SAMe can help alleviate them.
SAMe has been found to be safe and effective in the treatment of mild and moderate depression and, according to some accounts, to have a faster onset of action than conventional antidepressants. In a meta-analysis of forty-seven studies, SAMe produced a significant improvement in mood. SAMe treatment was significantly better than placebo. There are a number of studies directly comparing SAMe to tricyclic antidepressants, with eight studies showing equal benefits and dramatically fewer side effects caused by SAMe.
One uncontrolled trial administered doses of 800 to 3,600 mg per day to thirteen depressed patients with Parkinson's disease for a period of ten weeks. Eleven patients completed the study, and ten had at least a 50 percent improvement.
Little research has studied SAMe's treatment of severe depression, so it's unknown whether SAMe would have the same benefits as it's shown for mild to moderate depression. It may be a good first choice for older patients with other health challenges such as cardiovascular disease, Parkinson's disease, or dementia. Three published case reports have shown SAMe to have been used safely and effectively in children.
Because starting SAMe can cause nausea, I recommend starting with 200 mg twice daily for the first two days. Then increase to 400 mg twice daily on day three, then to 400 mg three times daily on day ten, and finally to the full dose of 400 mg four times daily on day fourteen. Other than possible mild gastric disturbance,
SAMe has no known toxicity. SAMe is expensive, so it may be a little toxic to the wallet.
Your body makes SAMe. There are no known food sources.
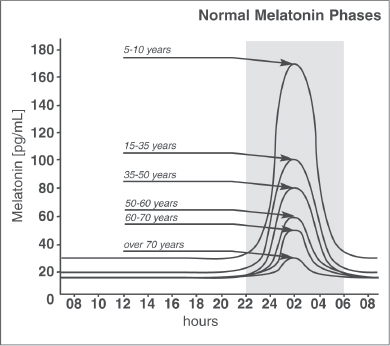
Figure
3: Peak Melatonin at Different Ages
A powerful antioxidant, melatonin is made by a small gland in the middle of your brain called the pineal gland, which secretes this hormone into your system when it gets dark outside. Low melatonin levels have been observed in patients with bulimia, fibromyalgia, breast cancer, and depression. Melatonin causes a surge in serotonin, which helps alleviate symptoms of depressive illness.
Melatonin's peak release is at night, but it's delayed in people with depression or panic disorder. This is called delayed sleep phase
syndrome (DSPS), which makes many depressed people want to stay up most of the night and sleep way too late into the day. If this describes you, you may need to work with melatonin and retraining your circadian rhythm.
People with episodic depression (mild depression that comes and goes) or seasonal affective disorder (SAD) (mild depression that correlates with fall and winter periods of shorter days with less daylight) have lower than normal melatonin levels. Small studies have proven these disorders to be successfully treated with melatonin.
If you are unable to sleep at night and wake up in the morning, then you may want to try the following plan.
- Thirty minutes before your eleven p.m. bedtime, take 1 mg melatonin and set your alarm for seven a.m.
- Wake at seven a.m. and take a supplement of adrenal support. I recommend one that has adrenal gland in it, which can help the body's natural morning rhythm get going. Many adrenal supports also contain vitamin B5 (pantethine) and eleutherococcus, a type of ginseng that is great for supporting adrenal function.
- Go for a walk outside in bright sunlight. If this is not possible, use a light box with 10,000 lux for thirty minutes.
- Turn to page 137 and read the list of symptoms treated by the homeopathic remedy staphysagria. If these describe you, take five pellets of a 30C dose once a day for two weeks.
These steps should help reset your circadian rhythm in about four weeks.
A common melatonin dosage may be anywhere from 0.5 to 6 mg, thirty minutes before bed. I usually suggest starting with 1 mg doses, and if you feel a bit groggy in the morning, you can lower
the dose. If 1 mg does not seem to help you fall asleep, you can increase the dose. Remember, if you have trouble staying asleep, you can work with tryptophan (see
chapter 3
) or a time-released melatonin, which sustains levels of melatonin throughout the night. Some studies have used very low doses of 0.125 mg in the late afternoon and evening. If you find the later dosing is not working for you, then try the low dose at four p.m. and eight p.m.
Side effects are rare as long as melatonin is taken thirty to forty minutes before a bedtime between ten and eleven thirty p.m. Some literature theorizes that melatonin might make people sadder. Although I have not seen this happen, it's a possibility, so listen to your body. Avoid taking melatonin if you have nighttime asthmatic symptoms.
