i bc27f85be50b71b1 (119 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown


VASCULAR SYSTEM AND HEMATOLOGY
389
Table 6-1-1. Differentiaring True Incerminent Claudication from
Pseudoc1audication
Charactcristic of
Incerminem
Discomfort
Claudication
Pseudoclaudication
Acrivity-induced
Yes
Yes or no
Location
Unilateral buttock,
Back pain and bilathip, thigh, calf and
eral leg pain
foar
Narure
Cramping
Same as with intermitlightness
tent claudication or
Tircdness
presence of tingling, weakness,
and clumsiness
Occurs with standing
No
Yes
Onset
Occurs at the same
Occurs at variable disdistance each time
tance each time
with walking on
with walking on
level surface
level surfaces
Unchanged or
Increased distance
decreased distance
when walking uphill
walking uphill
Unchanged or
Decreased distance
increased distance
walking downhill
walking downhill
Relieved by
Stopping activity
Sitting
Sources: Data from JR Young, RA Graor, j\'V Olin, JR Bartholomew (eds). Peripheral
Vascular Diseases. St. Louis: Mosby, 1991; 183; and JM Fritz. Spinal Stenosis. In JD
Placzck, DA Boyce (eds). Orthopacdic Physical Therapy Secrets. Philadelphia: Hanley
& Helfu,. 2001;344.
• Genetic abnormality in collagen (e.g., with Marfan's syndrome)
• Aging and natural degeneration of elastin
•
Increased proteolytic enzyme activity
• Atherosclerotic damage to elastin and collagen
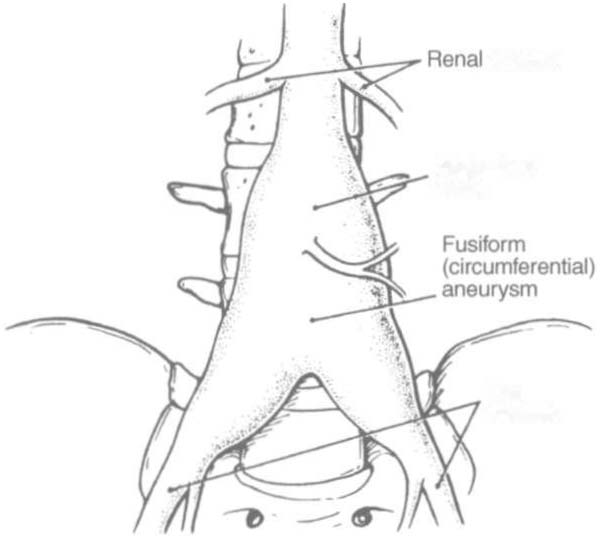
A true aneurysm is defined as a 500/0 increase in the normal diameter of the vessel" and involves weakening of all three layers of the arterial wall. True aneurysms are also generally fusiform and circum-




390 ACUTE CARE HANDBOOK FOR PHYSI AL THERAPISTS
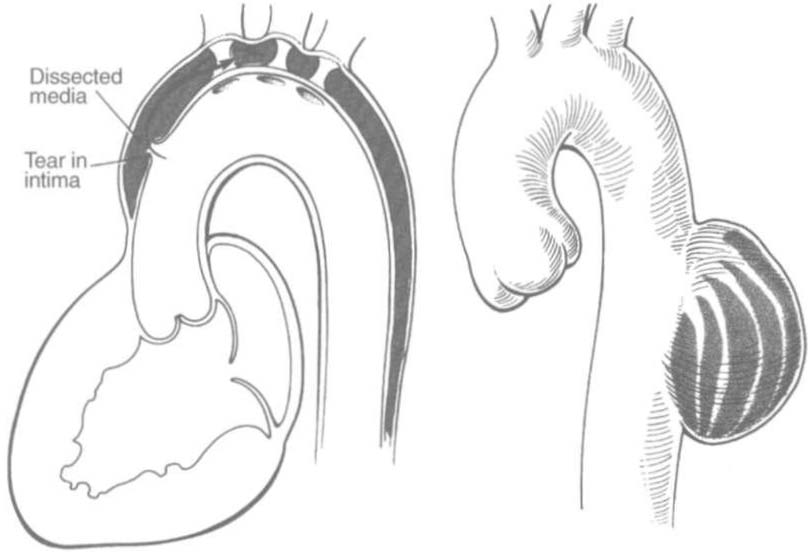
ferential in nature. False and saccular aneurysms are the result of
trauma from dissection (weakness or separation of the vascular layers) or clot formation. They primarily affect the adventitial layer."
Figure 6-2A and C demonstrate fusiform and saccular aneurysms,
and Figure 6-2B illustrates an arterial dissection.
Abdominal aneuryms may present with vague abdominal pain but
are relatively asymptomatic until an emboli dislodges from the aneurysm or the aneurysm ruptures 22 Aneurysms will rupture if the intraluminal pressure exceeds the tensile strength of the arterial wall.
The risk of rupture increases with increased aneurysm size.13
Clinical Tip
Abdominal aortic aneurysms are frequently referred to as
AAA or Triple A in the clinical setting.
The following are additional clinical manifestations of aneurysms:
•
Ischemic manifestations, described earlier, in Atherosclerosis, if
the aneurysm impedes blood flow.
• Cerebral aneurysms, commonly found in the circle of Willis,
present with increased intracranial pressure and its sequelae (see
General Management in Chapter 4 for more information on inrracranial pressure).!1
• Aneurysms that result in subarachnoid hemorrhage are also discussed in Chapter 4.
• Low back pain (aortic aneurysms can refer pain to the low
back).
• Dysphagia (difficulty swallowing) and dyspnea (breathlessness)
resulting from the enlarged vessel's compressing adjacent organs.
Surgical resection and graft replacement are generally the desired
treatments for aneurysms.2J However, endovascular repair of abdominal aneurysms is demonstrating favorable results. Endovascular repair involves threading an endoprosthcsis through the femoral
artery to the site of the aneurysm. The endoprosthesis is then attached
ro the aorta, proximal to the sire of the aneurysm, and distal, to the
iliac arteries. This effectively excludes the aneurysm from the circularion, which minimizes the risk of ruprure.22 Nonsurgical candidates must have blood pressure and anticoagulation managemenr.2J