i bc27f85be50b71b1 (59 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

Carpal Fractures
Carpal fractures and associated ligamentous injury or dislocation are
rypically due to compressive or hyperextension mechanisms of
injury.33 Management for the fracture of any carpal bone is similar.
Nondisplaced fractures are treated with short arm cast immobilization with the wrist positioned in neutral flexion-extension with slight ulnar deviarion.33 Displaced fracrures a re rreated with closed reduction and casring or ORIF wirh a postoperative splint or casr. Patients with isolated carpal fracrure are usually treared in rhe ambularory
care setting.
Clinical TIp
For patients who have concurrent lower- and upperextremity injuries and require the use of a walker or
crurches, a platform attachment placed on the assistive
device will allow weight bearing ro occur through the
upper extremity proximal to the wrist.
Metacarpal alld Phalallgeal Fractllres
Metacarpal fractures result from direct trauma, such as a crush injury,
or by long-axis loading, as with punching injuries. The fracture may be
accompanied by severe soft tissue injuries that can result in a treatment
delay of 3-5 days ro allow for a decrease in edema. Definirive trearment
depends on rhe locarion of the fracture-either the arricular surface

190 AClITE CARE HANDBOOK FOR PHYSICAL THERAPISTS
(ORIF), neck (closed reduction, percutaneous pinning, immobilization,
or a combination of these), shaft (ORlF, percutaneous pinning, immobilization, or a combination of these), or base (percutaneous pinning and immobilization) of the metacarpal.
Phalangeal fractures result from crush forces and consequently are
usually compounded by skin, tendon, and ligament damage. Management of nondisplaced phalangeal fracture is reduction and splinting.
Management of displaced or intra-articular fracture is OR1F with
splinting. Patients with isolated metacarpal and phalangeal fracture
are usually treated in the ambulatory care setting.
Joint Arthroplasty
Joint arthroplasty, the surgical reconstruction of articular surfaces
with prosthetic components, is indicated to restore function and
motion to a joint that is affected by degenerative arthritic changes."
Total joint arthroplasty is reserved for the individual with pain that is
no longer responsive to conservative measures, such as anti-inflammatory medication, restriction or modification of activity, exercise, weight loss, or the use of an assistive device. This surgery is elective in
nature and can be unilateral or bilateral. The incidence of bilateral
total joint arthroplasties, simultaneous or staged, being performed in
the acute care setting has increased in recent years. Bilateral joint
arthroplasty has been established to be a safe procedure that reduces
total rehabilitation time and hospital length of stay, thus decreasing
medical costs and length of debilitation of the patient.35
Joint arthroplasty provides patients and caregivers with a predictable postOperative course in the acute orthopedic care setting. For this reason, there are high expectations for these patients to achieve specific short- and long-term functional outcomes. The following sections provide basic surgical information and clinical techniques and suggestions for the acute care physical therapist.
Hip Arthroplasty
Hip arthroplasty involves the replacement of the femoral head, the
acetabulum, or both with prosthetic component . A hip arthroplasty
is most commonly performed on patients with severe hip arthritis
(degenerative or rheumatoid), AVN, hip infection, or congenital dis-

MUSCULOSKELETAL SYSTEM
191
Table 3-5. Hip Disorders That May Require Tara I Hip Arthroplasty
Degenerative arrhritis (hyperrrophic or osteoarrhritis)
Rheumaroid arthritis
Arraumatic avascular necrosis
Imrapelvic prorrusio acetabuli"
Congeniml subluxation or dislocation
Post-traumatic disorders (femoral neck, trochameric, or acetabular
fractures)
Failed reconstructive procedures (femoral osteotomy, arthrodesis, or
resurfacing)
Metabolic disorders (Paget'S disease, Gaucher's disease, or sickle cell
anemia)
Fused hip or ankylosing spondylitis
Infectious disorders (tuberculosis and pyogenic arthritis)
Bone tumors
Neurologic disorders (cerebral palsy and Parkinson's disease)
·Chronic progression of thc femoral head into rhe acetabulum and pelvis.
Source: Adapted from JW llarkcss. Arthroplasry of Hip. In ST Canale (cd), Campbell's
Opera rive Orthopaedics, Vol. 1 (9th cd). 51. Louis: Mosby, 1998.
orders. Refer to Table 3-5 for a complete list of hip disorders that may
require hip arthroplasty.
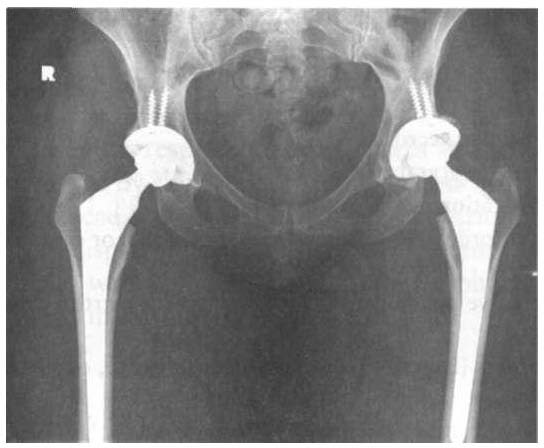
The 1110st common type of hip arthroplasty, a total hip arthroplasty
(THA), is the replacement of both the femoral head and the acetabulum with a combination of metal (titanium or cobalt alloys) and polyethylene components (Figure 3-13). Technology and research have introduced new materials for the weight-bearing components, such as
ultra-high-molecular-weight polyethylene and ceramic-on-ceramic and
metal-on-metal implants; however, long-term survival of such components is not yet known.36
The acetabular and femoral components may be tmcentenled or
cemented. Uncemenred components are commonly used in the
younger, active patient, as well as in a patient with a revision THA
involving a failed cememed prosthesis. The uncemented components
have areas of porous coated metal on the surface that may be treated
with a biochemical agent, hydroxyapatite, to promote bony ingrowth
for improved fixation.'7 Press-fit prostheses are also being used and
have heavily textured surfaces that achieve fixation through interference or interlocking of bone and metal surfaces." Use of uncemented