i bc27f85be50b71b1 (113 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown


366
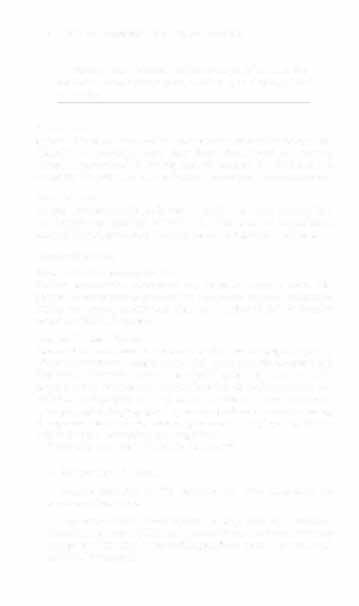
AClITE CARF HANDBOOK FOR l'HYSICAL TJ-IFRAPlqs
Table 6-3. Blood Cell Types
Cell
Description
Erythrocyte (red
Contains hemoglobin molecules responsible for oxygen
blood cell) (RBC)
rranspon w tissues.
Composed of four protein chains (two alpha and twO
beta chains) bound w four iron pigment complexes.
An oxygen molecule attaches ro each iron J,wm W
become oxyhemoglobin.
Leukocyte (whire
Five types of \�'BCs (neutrophils, basophils, eosinophils,
blood cell) (WBC)
lymphocytes, and monocytes) are responsible for
launching immune defenses and fighting infection.
WBCs leave the circulation [0 gain access to a site of
infection.
Thrombocyte
Cell fragment responsible for dar formarian.
(platelet)
Source: Data from The Cardiovascular System: Blood. In EN Maricb, Human AnalOmy
and Physiology (3rd cd). Redwood City, CA: Bcnjamm·Cummings, 1995.
2.
The transport of carbon dioxide and merabolic waste
products to the lungs and kidneys, respectively
3.
The rransport of hormones from endocrine glands to tar-
get organs
4.
The maintenance of body temperature via conduction and
dispersal of heat
5.
The maintenance of pH with buffers freely circulating in
the blood
6.
The formation of clots
7.
The prevention of infection with white blood cells
(WBCs), antibodies, and complement
The vascular and hematologic systems are intimately linked, and
the examination of these systems is often similar. For the purpose of
this chapter, however, the evaluation of the vascular and hematologic
systems is discussed separately.



VASCULAR SYSTEM AND HEMATOLOGY
367
Physical Examination
Vascular Evalt/atio"
History
In addition to the general chart review (see Appendix I-A), the following information is important to gather during the examination of the patiem with a suspected vascular disorder]:
• Relevant medical history that includes diabetes mellitus, hypertension, syncope or vertigo, and non healing ulcers.
• Relevant social history that includes exercise and dietary habits,
as well as the use of tobacco or alcohol.
• Presence of intermittent claudication (leg pain that occurs with
walking). When (onset) and where (location) does it OCCUt, and
what makes it better?
• Presence or history of peripheral edema. Is it acute or chronic? If
chronic, what is the patient'S baseline level of edema?
•
Precautions, such as weight bearing or blood pressure parameters after vascular surgery.
Clinical Tip
Intermittent claudication is often abbreviated in the clinical setting as Ie.
Inspection
Observation of the following features can help delineate the location
and severity of vascular disease and help determine whether these
manifestations are arterial or venous in origin i.]:
• Skin color. (Note the presence of any discoloration of the distal
extremities, which is indicative of decreased blood flow---e.g.,
mottled skin.)
• Hair distribution. (Patchy hair loss on the lower leg may indicate arterial insufficiency.)

368
AClJrE CARE HANDBOOK FOR PHYSICAL THERAPISTS
•
Venous pattern (dilation or varicosities).
•
Edema or atrophy. (Peripheral edema from right-sided congestive heart failure occurs bilaterally in dependent areas; edema from trauma, lymphatic obstruction, or chronic venous
insufficiency is generally unilateral.) Refer to Table 1-6, Pitting
Edema Scale.
•
Presence of cellulitis.
•
Presence of petechiae (small, purplish, hemorrhagic Spots on
the skin).
•
Skin lesions (ulcers, blisters, or scars).
•
Digital clubbing (could be indicative of poor arterial oxygenation or circulation).
•
Gait abnormalities.
Palpation
During the palpation portion of the examination, the physical
therapist can assess the presence of pain and tenderness, strength
and tate of peripheral pulses, respiratory rate, blood pressure, skin
temperature, and limb girth (if edematous). Changes in heart rate,
blood pressure, and respiratory rate may correspond to changes in
the fluid volume status of the patient. For example, a decrease in
fluid volume may result in a decreased blood pressure that results
in a compensatory increase in heart and respiratory rates. The
decreased fluid volume and resultant increased heart rate in this
situation may then result in a decreased strength of the peripheral
pulses on palpation. In patients with suspected or diagnosed
peripheral vascular disease, monitoring distal pulses is more
important than monitoring central pulses in the larger, more proximal vessels.3
The following are twO systems used to grade peripheral pulses:
1.
On the scale of 0-3 as'
0 Absent
+1 Weak and thready pulse
+2 Normal
+3 Full and bounding pulse

VASCULAR SYSTEM AND HE.MATOLOGY
369
2.
On rhe scale of 0-4 as'
0
Absent
1
Markedly diminished
2
Moderately diminished
3 Slightly diminished
4
Normal
Peripheral pulses can be assessed in the following arteries (see
Figure 1-6):
• Temporal
• Carotid
• Brachial
• Ulnar
• Radial
• Femoral
• Popliteal
• Posterior tibial
• Dorsalis pedis
Clinical Tip
• Peripheral pulse grades are generally denoted in the
medical record by physicians in the following manner:
dorsalis pedis +1.
• A small percentage of the adult population may normally have absent peripheral pulses-for example, 10-
17% lack dorsalis pedis pulses.'
•
In patients who have disorders resulting in vascular
compromise (e.g., diabetes mellitus, peripheral vascular
disease, or hypertension), pulses should be monitored
before, during, and after activity not only to determine
any rate changes, but, more important, to determine any
changes in the strength of the pulse.
370
ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
•
Notation should be made if the strength of pulses is correlated to complaints of pain, numbness, or tingling of the
