i bc27f85be50b71b1 (245 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown


AI'I'ENDIX III-A: ,"IEDICAL-SURGICAL EQUIPMENT IN THE ACUTE CARE SETTING
781
Figure IlI-A.S. Nonrebreather mask. (Maersk Medical, Respiratory and
Anesthesia Product Catalog, McAllen, TX.)
flowing as indicated, and that the cannula or mask is properly
positioned .
•
The 0, system may need added humidification, as supplemental 0, may be drying to the nasal mucosa and lead to nosebleeds (epistaxis); however, added humidification is contraindi-cated in
several systems, as indicated in Table III-A.] and Table III-A.2.
•
Provide extra lengths of 0, tubing if functional mobility will
occur farther than 5 or 6 ft from the bedside (i.e., the wall 02
source).

782 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Aerosol
Hood
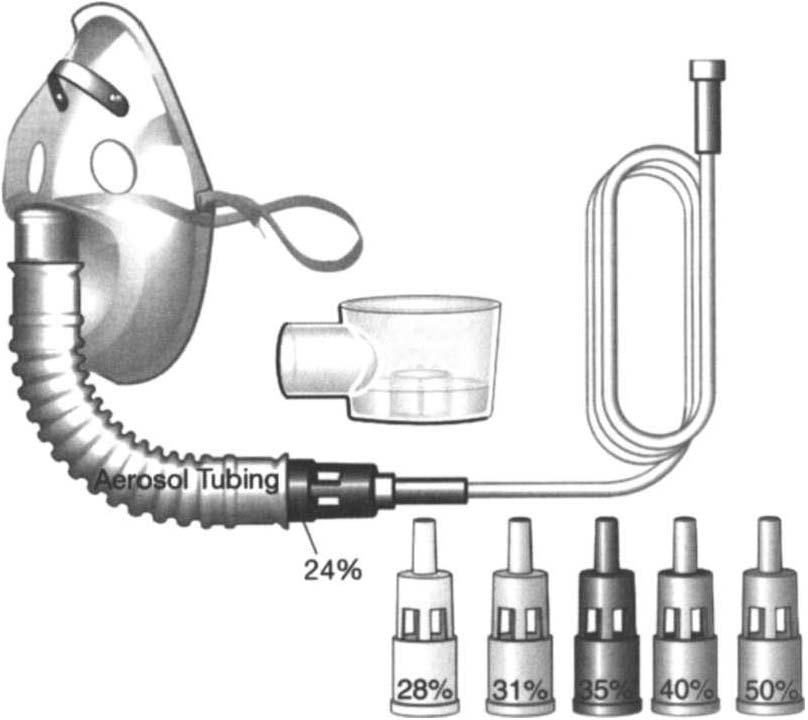
Figure [I]-A.6. Air e"trainment mask or venturi mask. (Maersk Medical, Resptratory and Anesthesia Product Catalog, McAllen, TX.)
•
Ensure that portable 02 tanks are rurned on and have sufficient
levels of 02 before use. Have back-up tanks available.
•
Observe masks for the accumulation of mucus or clogging.
Clear or change the cannula or mask if needed.
•
Monitor the patient's skin for potential breakdown due to pressure from the cannula or mask. Provide appropriate padding without interfering with the fit of the cannula or mask.
•
Document the type and amount of supplemental 02 used during
physical therapy intetvention.

AI)I)ENDIX III-A: MEDICAL-SURGICAL EQUIPJ'"tENT IN THE AClITE CARE SETTlNC
783
Hemodynamic Monitoring
Monitoring hemodynamic events provides information about the
adequacy of a patient's circulation, perfusion, and oxygenation of
the rissues and organ sysrems. The goal of hemodynamic moniroring
is to maintain rhe balance berween oxygen demand and oxygen
delivery.' Hemodynamic monitoring can be accomplished using
noninvasive (Table III-A.3) or invasive (Table III-A.4) merhods.
Noninvasive, or indirect, hemodynamic monitoring provides
physiologic information without the risks of invasive monitoring
and can be used in many serrings; however, the accuracy of the
dara obrained is affected by the applicarion of rhe device and the
comperence of rhe clinician gathering the data.s
Invasive, or direct, measurements are obtained by penetration
of the skin and insertion of a cannula or carheter into a blood vessel, chamber of rhe heart, or borh. The cannula or catheter is attached to a monitoring system, which consists of a transducer,
amplifier, and oscilloscope for rhe display of rhe vascular waveforms and pressure measurements.9 Direct monitoring can provide continuous, accurate data; however, thrombosis, infections, air
embolisms, and trauma are potential complications.s
During invasive hemodynamic moniroring, the level of rhe righr
atrium is the standard zero reference point and is identified by the ph/ebosratic axis-the intersection of rhe midaxillary line and the fourth inrercosral space (see Figure In_A.7).'O The nurse will zero the system
using a level to align the patient's phlebostatic axis with the transducer.
Repositioning the patient may artificially alter waveforms by applying
pressure to the catheter, shifting the catheter or stopcock, or shifting the
phlebostatic axis relative ro the transducer. I I
General Physical Therapy Considerations with
Hemodynamic Monitoring
•
Raising rhe level of the phlebostaric axis relarive to rhe transducer gives false high readings; lowering rhe phlebosratic axis gives false low readings."
•
If a waveform changes during treatment, in the absence of other
clinical signs, reposition the patient or limb (if an arterial line is in
place) and reassess. If rhe waveform does nor rerum to baseline,
rhen notify the nurse.


Table ill-A.3. Noninvasive Medical Monitoring
....
00
...
Device
Description
Clinical Implications
>
g
BP cuff (sphygmomanometer)
P urpose: indirectly measures arterial
•
Do not use a BP cuff on an extremiry with an
'"
Normal adult values: systolic
blood pressure.
arterial line, lymphedema, AV fistula or graft,
�
�
'"
100-J 40 mm Hg, diastOlic
'"
�
Consists of: an inflatable cuff, usually
or blood clot, or in an extremity ipsilateral CO a
60-90mm Hg
placed 2.5 em proximal to the
mastectomy. Try to avoid measuring SP in an
J:
>
z
antecubital space, attached to a
extremiry with a peripheral or central intra
"
pressure monitoring device.
venous line. Look for signs posted at the
1')
o
Auscultate for Kororkoff's sounds
patient's bedside stating whether the use of a BP
"
(refer to Table 1-8) with a
cuff on a particular extremity is contrindicated.
o
'"
stethoscope over an artery, usually
•
Use an appropriately sized cuff. The cuff
:t
the brachial artery.
bladder should be no less than 80% of limb
-<
�
circumference. A cuff that is roo small
r;;
overestimates SP.
r
J!
•
The cuff may be placed on the upper extremity
distal to the elbow with auscultation of the
iii
>
�
radial artery.
�
•
Alternative sites for measurement in the lower
extremiry are proximal to the popliteal space
with auscultation of the popliteal artery or
proximal to the ankle with auscultation of the
posterior tibial artery.
•
Avoid contact between stethoscope tubing and
the cuff robing to minimize extraneous sounds.


