i bc27f85be50b71b1 (50 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

position, and skin integrity.
Posture
Observe the patient's resting posture in supine, sitting, and standing
positions. This includes inspection of the head, trunk, and extremities
for alignment, symmetry, deformity, or atrophy.
Limb Position
Observe the resting limb position of the involved extremiry. Compare to both normal anatomic position and to the contralateral side.
Note if the limb is in position naturally or if it is supported with a
pillow, roll, or wedge.
Clinical Tip
• A limb in a dependent position is at risk for edema
formation, even if it is dependent for only a short period
of time.
• Maintain joints in a neutral resting position to preserve
motion and maintain soft tissue length.
Skin Integrity
The patient'S skin integrity should be inspected in general for edema,
discoloration, bruising, or scars. If there is traumatic injury, carefully inspect the skin at the level of and distal to the injury. Note any lacerations or abrasions. If the patient has recently had surgery,
observe the location, direction, and quality of incision(s}. Note any
pressure sores or potential for such. Refer to Chapter 7 for further
discussion of skin integrity evaluation.

MUSCULOSKEU:.iAL SYSTEM
163
Clinical Tip
Pressure sores from prolonged or increased bed rest after
trauma or orthopedic surgery can develop in anyone,
regardless of age or previous functional abilities. Inspect
the uninvolved extremity for skin breakdown too.
Palpatio1l
Palpate skin temperature to touch, capillary refill, and peripheral
pulses at the level of or distal to injury or the surgical site. Refer to
Chapter 6 for further discussion of vascular examination. A discussion of special tests is beyond the scope of this text; however, the therapist should perform special testing if results of the interview or screening process warranr further investigation.
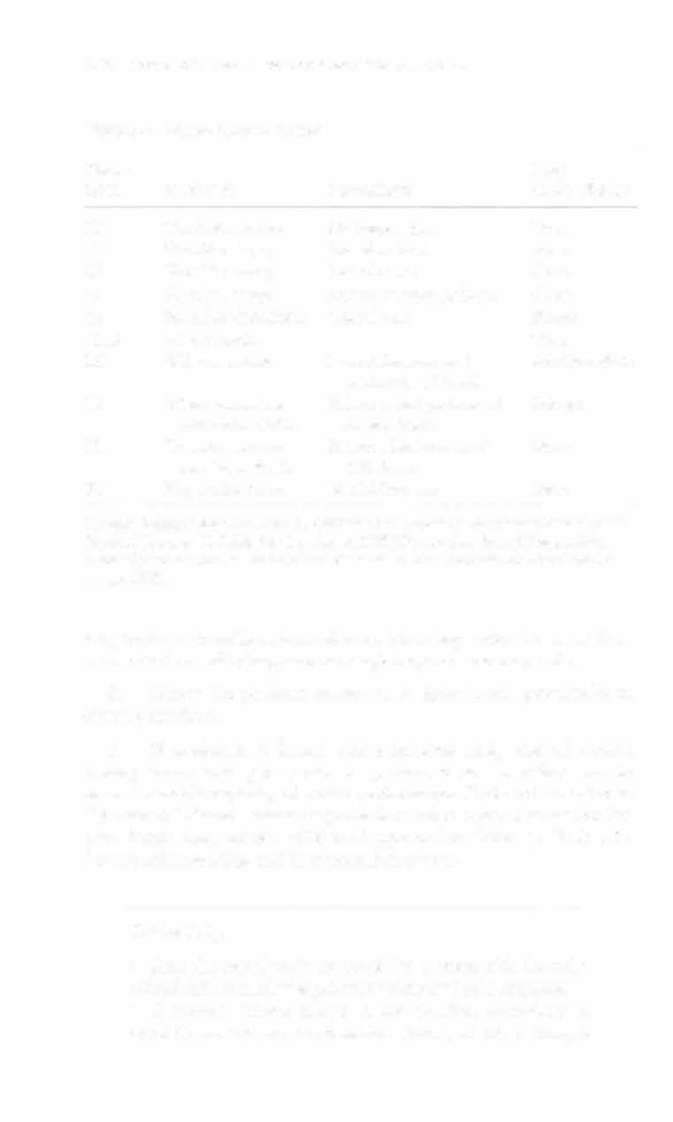
Upper- a1ld Lower-Qllarter Screens
Upper- and lower-quarter screening is the brief evaluation of bilateral
range of motion (ROM), muscle strength, sensation, and deep tendon
reflexes. It is a very efficient examination of gross neuromuscular status that guides the therapist to perform more specific testing.' The therapist should perform both an upper- or lower-quarter screen,
regardless of the extremity involved. For example, for a patient with
lower-extremity involvement who will require the use of an assistive
device for functional mobility, both functional range and strength of
the upper extremities muSt also be assessed. Tables 3-1 and 3-2
describe a modified version of an upper- and lower-quarter screen.
Table 3-3 outlines normal ROM. Peripheral nerve innervations for
the upper and lower extremities are listed in Tables 4-7 and 4-8,
respectively. Dermatomal innervation is shown in Figure 4-6.
The sequencing of the upper- and lower-quarter screen is as
follows2:
1.
Observe active ROM and test myotomes progressing from
proximal to distal and beginning at the spinal level and moving dis-




164 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
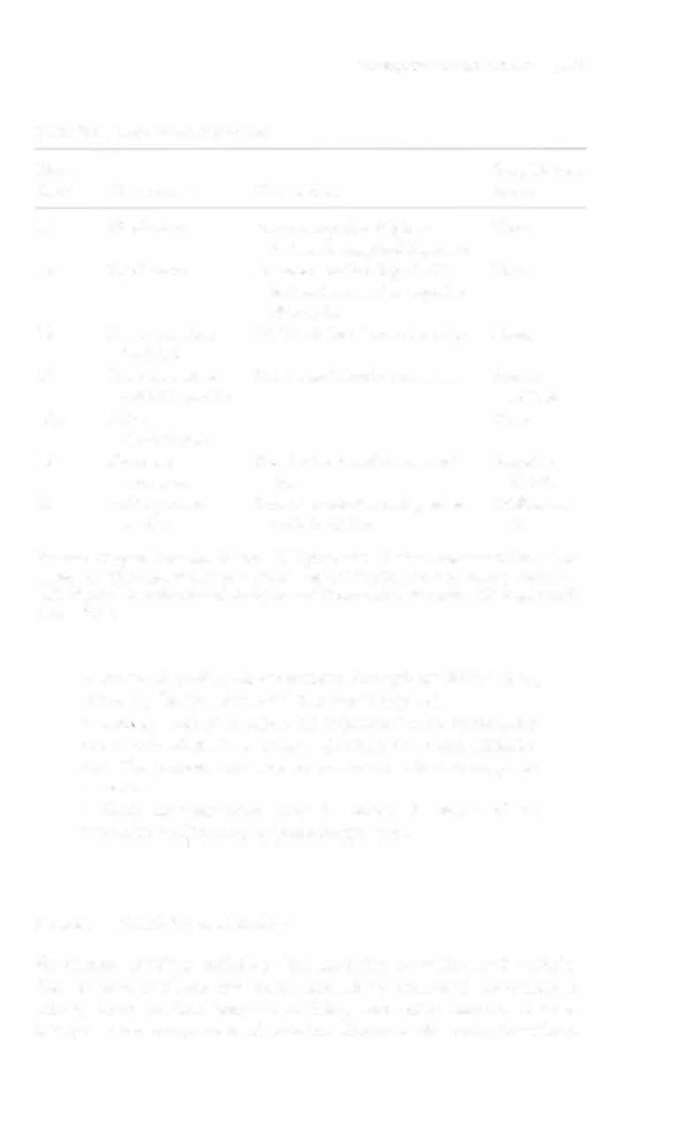
Table 3-l. Upper-Quarter Screen
Nerve
Deep
Root
Mymome
Dermatome
Tendon Reflex
CI
Cervical rmation
No innervation
None
C2
Shoulder shrug
Posterior head
None
C3
Shoulder shrug
Posterior neck
None
C4
Shoulder shrug
Acromioclavicular joint
None
C5
Shoulder abduction
Lateral arm
Biceps
C5,6
Elbow flexion
None
C6
Wrist extension
Lateral forearm and
Brachioradialis
palmar tip of rhumb
C7
Elbow extension
Palmar distal phalanx of
Triceps
and wrist flexion
middle finger
C8
Thumb extension
Palmar distal aspect of
None
and finger flexion
litde finger
Tl
Finger abduction
Medial forearm
None
Sources: Adapted from ML Palmer, ME Epler (cds). Clinical Assessment Procedures in
Physical Therapy. Philadelphia: Lippincort, 1990;32; and dara from S Hoppenfeld.
Physical Examination of [he Spine and Extremities. East Nor""alk, Cf: Appleton &
Lange, 1976.
tally to the extremities. Remember that it is imperative to assess these
below the level of injury, as neurologic impairments may exist.
2.
Screen the patient's sensation to light touch, proximally to
distally, as above.
3.
If weakness is found, assess strength using manual muscle
testing. Break testing may also be performed as a modified way to
assess isometric capacity of motor performance. If altered sensation to
light touch is found, assess deep touch or other types of sensation further. Assess deep tendon reflexes if apptopriate. Refer to Table 4-15
fot the reflex grading and interpretation system.
Clinical Tip
• Start the examination or screening process with the uninvolved side to minimize patient anxiety and pain response.
• If manual muscle testing is not possible secondary to
conditions such as altered mental status, describe strength