i bc27f85be50b71b1 (65 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

208 AClJTE CARE HANDOOOK FOR PHYSICAL THERAPISTS
Figure 3·19. Total hip arthroplasty resection (Girdlestone).
Physical Therapy Intervention after Resection Arthroplasty
Physical therapy after a resection arthroplasty withollt reimplantation or a two-staged reimplantation is dependent on the extent of joint or bone destruction caused by the infection and the removal
of the prosthetic components, cement, and debridement of soft tissue. Weight-bearing restrictions may depend on use of cement spacers and vary from non weight bearing to weight bearing as tolerated, as established by the surgeon. Physical therapy sessions focus on functional mobility, safety, assistive device evaluation,
and maintenance of muscle strength and endurance in anticipation
for reimplantation of the joint.
• Patients who have an infection and joint resection arthroplasty
may be compromised by general malaise and decreased endurance
secondary to the infection, and, possibly, from increased blood loss
during surgery. This may lead to decreased pain tolerance. The
physical therapist should take these factors into account when
mobilizing the patient. Functional mobility training should begin
when the patient is stable, and physical therapy sessions should be
modified for patient tolerance.
• THA precautions often do not pertain after removal of the prosthesis. The physical therapist should verify any other precautions, such as trochanteric precautions (see Table 3-6) and weight-bearing status,

MUSCULOSKELETAL SYSTEM
209
with the surgeon. Without movement precautions, most isometric,
active, and active-assisted exercise may be appropriate. Progress the
patient as tolerated to maximize function, strength, and endurance in
preparation for eventual reimplantarion of the prosthesis.
• For knee resection surgery, strengthening exercises for the quadriceps muscle can be initiated as long as the extensor mechanism is intact. Isometrics, active-assisted, and active-straight leg raises can
be initiated according to patient comfort.
• Edema should be controlled with ice and elevation. Positioning
of the limb is important to decrease discomfort from muscle spasm
and the potential for deformities caused by muscle contractures
around the hip and knee.
Clinical Tip
• A hip Girdlestone procedure may leave a patient with a
significant leg-length discrepancy. A patient'S shoes should
be adapted with a lift to correct gait and increase weight
bearing on the affected extremity.
•
With decreased leg length, the musculature surrounding
the hip shortens. External (e.g., Buck) traction can be used
to maintain muscle length and may be used while the
patient is in bed. Shortened muscles may spasm. Isometric
exercises should be encouraged to gain control of these
muscles to reduce spasm.
• ROM should be minimal with knee resection so as to
maintain integriry of bone surfaces if reimplantation is
planned. A brace or knee immobilizer should be worn during functional activities to maintain knee extension but
can be removed in bed. The unaffected limb can assist
with lifting the affected limb with transfers out of bed.
• With a patient that is non weight bearing, a shoe on the
unaffected side and a slipper sock on the affected side can
assist with roe clearance when advancing the affected leg
during the swing phase of gait. Conversely, with a patient
who has a significant leg-length discrepancy, a slipper sock
on the unaffected side and a shoe on the affected side can
assist with ambulation until a shoe lift is obtained.

2 1 0
ACUTE. CARE HANDBOOK FOR PHYSICAL THERAPISTS
Surgeries of the Spine
The vertebral column fotms the central axial suppOrt of the body and
consists of bony segments and fibrocartilaginous discs connected by
ligamentous structures and supportive musculature. Degenerative,
traumatic, or congenital changes can cause compensation in the vertebral bodies, intervertebral discs, facets, and interverrebral foramen.
Any changes in these struc[Ures can result in dysfunction that, in turn,
causes pain. Some common dysfunctions of the spine and associated
structures are ligamentous sprain, muscle strain, herniated nucleus
pulposus, rupture of the intervertebral disc, spinal stenosis with nerve
root compression, spondylolisthesis, and degenerative disease of the
disc, vertebral body, or facet joints. Any dysfunction can present itself
in the cervical, thoracic, and lumbar spine.
Back pain is the major indication for spinal surgery. Pain can be
disabling ro a patient, limiting the ability to work or complete ADLs.
Any acute injury, such as muscle spasm, herniated nucleus pulposlls,
and chronic low back pain exacerbations, should be managed conservatively before surgical treatment is recommended. Many injuries will heal with treatments, such as bed rest, anti-inflammatory medication,
lifestyle modification, education in proper body mechanics, and outpatient physical therapy.56 Surgery may be indicated when rhese measures fail to relieve a patient'S symptoms or if there is a decline in the neurologic status of the patient.
Advances have been made in all areas of spinal surgery; however,
there is still no cure for low back pain. Low back pain and leg pain
can arise from degenerative disc disease and herniation or rupture of
the intervertebral disc. Surgical procedures can be performed to
relieve the symptoms associated with degenerative disc disease when
conservative measures have failed. Open disc surgery and microdiscecromy remove disc fragments and herniated disc material that compress the adjacent nerve root. Microdisceclomy is a minimally invasive procedure that uses a microscope to view the surgical area,
allowing for decreased surgical exposure '6 Most microdiscectomy
surgery can be done on an outpatient basis, and early return to activity can be accomplished. Symptom relief is high both inirially postoperatively and on a long-term basis.57 If additional exposure of the nerve root is needed, associated procedures, such as a laminectomy or
foraminoromy, may be performed in conjunction with discectomy or
spinal fusion. Refer ro Table 3-8 for descriptions and indications for
these procedures.

MUSCULOSKt::LI:.'AL SYSTEM
21 t
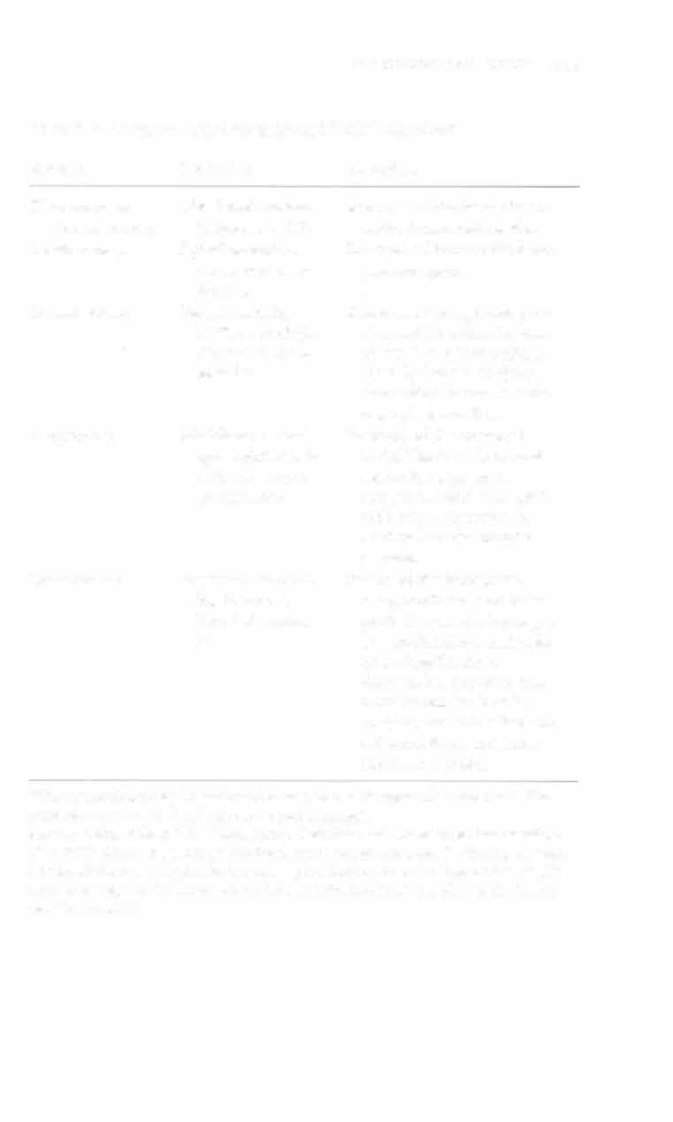
Table 3-8. Common Spinal Surgeries and Their Indications·
Surgery
Indication
Procedure
Discectomy or
Herniated nucleus
Removal of the herniation or
microdiscecromy
pulposus (HNP)
entire intervertebral disc.
Laminecromy
Spinal stenosis or
Removal of bone at the internerve root comlaminar space.
pression
Foraminotomy
Spinal stenosis,
Removal of the spinous pro
HNP, or multiple
cess and the entire laminae
nerve roOt comro [he level of the pedicle.
pression
Usually done in conjunction with a fusion to maintain spinal stability.
Carpectomy
Multilevel stenosis,
Removal of the vertebral
spondylolisthesis
body. The disc above and
with nerve root
below the segment is
compression
removed, and a strut graft
with instrumentation is
used to fuse the anterior
column.
Spinal fusion
