Read Oxford Handbook of Midwifery Online
Authors: Janet Medforth,Sue Battersby,Maggie Evans,Beverley Marsh,Angela Walker
Oxford Handbook of Midwifery (67 page)
- Lidocaine can be injected slowly as the needle is withdrawn. However,
 it is considered to be more effective if 3–4mL are injected initially and
it is considered to be more effective if 3–4mL are injected initially andthen, before removing the needle, the remaining lidocaine is injected
either side of the initial injection, in a fan shape.
- At least 4–5min must be given for the analgesic to be effective prior to incision (Fig. 14.3).
- Use blunt-ended scissors.
- Insert two fingers into the vagina, as before.
- Lidocaine can be injected slowly as the needle is withdrawn. However,
PERFORMING AN EPISIOTOMY
281
- Open the blades of the scissors; insert the blade accessing the vagina flat over the fingers, and then rotate into the cutting position with the outer blade.
- Make a cut of approximately 4cm within the anaesthetized area.
- Cut concisely and deliberately at the height of a contraction, when the perineum is maximally stretched, to minimize bleeding and pain.
- A medio-lateral incision is commonly used or sometimes a ‘J’ shaped incision. Both methods help to prevent extension of the incision to the anal sphincter.
- Preparation for an imminent delivery is important. It is vital to deliver the head carefully and prevent the shoulders being expelled before restitution has occurred.
- If the delivery is delayed, control bleeding by applying pressure to the episiotomy.
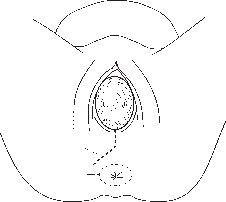
Line of incision Anal sphincter

Fig. 14.3
Episiotomy.1
Carroli G, Belizan J (2006). Episiotomy for vaginal birth (Cochrane review). In:
Cochrane Library
, Issue 3. Chichester: John Wiley and Sons.CHAPTER 14
Normal labour: second stage282
Female genital mutilation
Female genital mutilation (FGM), also known as female circumcision, is deeply rooted in the traditions and religion of about 30 countries. In the UK it is most commonly seen amongst immigrants from Somalia, Eritrea, Mali, Sudan, Ethiopia, Sierra Leone, and Nigeria. The practice has been outlawed in the UK, and parents found to be carrying out this practice, or returning to their country of origin for this to be undertaken, are at risk of severe penalties.
Definition
FGM involves a variety of invasive procedures that result in partial or total removal of the external female genitalia and/or other injury to the female genital organs, for cultural or any other non-therapeutic reason.
Classification
- Type 1: excision of the prepuce, with or without excision of part or all of the clitoris.
- Type 2: excision of the prepuce and clitoris, together with partial or total excision of the labia minora.
- Type 3: excision of part or all of the external genitalia and stitching/ narrowing of the vaginal opening (infibulation).
- Type 4: unclassified: includes pricking, piercing, or incision of the clitoris and/or labia; stretching of the clitoris and or labia; cauterization by burning the clitoris and surrounding tissues; scraping of the vaginal orifice or cutting the vagina; introduction of corrosive substances to the vagina to cause bleeding, or herbs placed in the vagina to cause tightening or narrowing of the vagina; any other procedure that falls under the above definition.
Cultural and historical background
- Most parents believe they are doing their best for their daughters and that they are adhering to sound cultural practices.
- A circumcised woman is regarded as spiritually pure and clean. An uncircumcised woman is regarded as shameful and unnatural by society and therefore not fit to marry or have children.
- It is believed she must undergo this procedure in order for her to identify with the everyday hardships of being a woman.
- Religious reasons—some women see it as a religious obligation. There are no references in the Bible or the Koran referring to FGM.
- It is claimed to promote chastity and virginity.
- It negates sexual pleasure.
- It is advocated as improving fertility and preventing maternal and infant
 mortality. The opposite is true, FGM puts the health of the woman and
mortality. The opposite is true, FGM puts the health of the woman andthe baby at great risk during pregnancy and childbirth.
- It is claimed to ensure that a woman is faithful to her husband, thereby preventing promiscuity.
- It is believed to promote cleanliness.
- Parents believe that FGM ensures a good marriage for their daughters.
Prevalence
FGM is commonly performed on girls between the ages of 4 and 10 years, but may also be performed soon after birth, at adolescence, at the time of
FEMALE GENITAL MUTILATION
283
marriage, or during the first pregnancy. The procedure is usually carried out by a traditional midwife or a woman within the local community. FGM is practised widely on the African continent, with countries such as Somalia and Sudan performing infibulation on 90–98% of girls. The WHO estimates that over 120 million women from 30 different countries have undergone FGM.
Complications
Following FGM, immediate complications are haemorrhage, pain, shock, infection, urine retention, injury to surrounding tissue, ulceration of genital area, and death. Long-term complications include:
- Type 1: excision of the prepuce, with or without excision of part or all of the clitoris.
- Delayed wound healing, keloid formation, and severe scarring
- Pelvic infection, recurrent urinary tract infection
- Formation of epidermoid cysts and abscess
- Neuromata
- Haematocolpos—vaginal closure leading to scarring can impair the flow of menstrual blood and exacerbate dysmenorrhoea
- Trauma and fears during childbirth
- Painful coitus
- Infertility
- Psychological trauma.
Complications during labour and birth
- Prolonged obstructed labour, due to tough scar tissue formation commonly found in type 3 FGM. Clitoridectomy does not cause obstructed labour.
- Perineal laceration.
- Uterine inertia, due to prolonged labour.
- Fetal distress caused by obstructed labour; may lead to fetal death (a common occurrence in Africa).
- Postpartum wound infections.
- Re-infibulation is commonly practised in Africa but is outlawed in the UK. Where possible, it is important to identify women who may have been subjected to FGM early in pregnancy, by asking sensitive but leading questions. In an area with a high ratio of African residents there may well be a specialist midwife. Reversal of infibulation can be carried out at about 20 weeks to allow for complete healing prior to labour. This will also provide access to the urethra and vaginal orifice during labour. However, some women prefer to have reversal performed during labour, so that the pain of de-infibulation is combined with the pain of labour. Adequate pain relief is crucial so that the woman is not further traumatized by the procedure. With the woman’s consent, an anterior midline incision that
exposes the urethra and clitoris (which is often buried under scar tissue)

is performed during labour. Prompt assessment of suturing requirements following birth should be attended to, and sensitive follow-up care of the woman’s physical and psychological welfare should be ongoing.
Recommended reading
Momoh C (ed.) (2005).
Female Genital Mutilation
. Abingdon: Radcliffe Publishing Ltd.CHAPTER 14
Normal labour: second stage284
Conduct of normal vaginal delivery
If a woman and her birthing partner have established a good rapport with their midwife, the environment is peaceful and unhurried, there is low lighting and privacy, with good communication and information, then the woman is likely to have a positive and empowering experience of birth.
The woman should be enabled to adopt a position for birth that she feels comfortable with, and should be relaxed enough to verbalize (shouting, grunting, etc.) to relieve tension and anxiety and to prevent breath-holding.
Preparation
- When birth is anticipated, put on protective glasses (in case of blood spillages).
- Wash your hands thoroughly, put on protective wear and gloves, and prepare the necessary equipment. A sterile area for equipment will need to be organized and accessible.
- The immediate birthing area should be prepared, e.g. mattress, birthing chair, etc.
- Prior to the birth, wash the vulva with water/lotion, drape sterile towels around the immediate area, and place a sterile pad over the anus to prevent faecal contamination.
- If the woman is in an upright position, the anal area will need to be kept free from faecal material.
Delivery
- Encourage the woman to work with her contractions as before.
- At crowning, encourage her to breathe gently and/or to pant her baby’s head out in a slow and controlled way. This helps to minimize perineal trauma, empowers the mother’s experience, and prevents the need for too much hands-on intervention.
- Be ready to prevent sudden delivery of the head. There is no physiological rationale for the application of firm pressure and resistance to maintain flexion, which serves only to increase the diameters of the fetal skull (b see Flexion technique, p. 277).
- Encourage the mother, both verbally and by non-verbal communication. This is crucial in helping to maintain her efforts and confidence. Make plenty of eye contact and give her praise, using a quietly spoken and supportive tone throughout.
- The Ritgen manoeuvre is generally not required if the birth is proceeding normally. Grasping the parietal eminences to overextend the head serves only to increase the diameters of the fetal skull (b see
 Care of the perineum, pp. 276–8).
Care of the perineum, pp. 276–8). - Checking for the cord around the neck of the baby can cause considerable discomfort for the woman, and opinions are mixed as to whether this procedure is routinely necessary.
- If the cord is around the neck, it can usually be untangled following delivery.
- If the cord is very tight, some suggest cutting the cord: two pairs of artery forceps are applied 2.5cm apart and the cord cut between
CONDUCT OF NORMAL VAGINAL DELIVERY
285
them, using cord scissors, and then unwound. However, this can often be a difficult procedure and may result in lower Apgar scores.
- Others suggest that cutting the cord is unnecessary, as the baby will be born through the loops of cord.
- Others suggest that cutting the cord is unnecessary, as the baby will be born through the loops of cord.
- If the cord is around the neck, it can usually be untangled following delivery.
- When birth is anticipated, put on protective glasses (in case of blood spillages).
Other books
The Witch and the Wolf: Part Two by Lola Kidd
In My Dreams by Renae, Cameo
Behindlings by Nicola Barker
Stripped Bare by Kalinda Grace
Braden: A Dark Mafia Romance by York, Adora
Tomorrow Is Too Far by James White
Stir It Up by Ramin Ganeshram
Breaking Bamboo by Tim Murgatroyd
Undercurrents by Robert Buettner
Sirius by Jonathan Crown

