Pediatric Primary Care Case Studies (55 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

The goal of CBT is to decrease negative schema and their emotional and behavioral consequences. This is done by: 1) assisting the individual to attempt new behaviors and experiences; 2) acknowledging the individual’s past but focusing the intervention on the present desired functioning; 3) viewing the changes in emotions and behavior from both an objective and subjective vantage point; 4) refocusing the individual on recent successful experiences; and 5) redirecting the self-evaluations to reasoned depictions of positive perceptions, beliefs, and attitudes. Problems that are brought to the therapy appointment are broken down into a series of questions, the answers to which gradually reveal the solution. In the session, the teen is asked to begin to question his or her own reactions. For example:
• What other plausible perspective(s) can I take about this matter?
• What factual evidence supports or refutes my beliefs?
• What are the pros and cons of continuing to see things the way I see them, and what are the pros and cons of trying to see things differently?
• What constructive action can I take to deal with my beliefs or schemas?
• What sincere advice would I give to a good friend with the same beliefs?
In any type of therapy it is difficult to understand numerous problems in their entirety. CBT focuses on individual events or problems and allows the therapist to conceptualize connections and solutions. A prioritization needs to occur in CBT, as follows: First, assess and problem solve for suicide risk. Next, address interfering behaviors such as homework noncompliance, medication noncompliance, not working collaboratively in therapy, and missing appointments. Third, address behaviors that are dangerous and that interfere with quality of life such as substance abuse, shoplifting, high-risk sexual behaviors, abusive relationships, or homelessness. These behaviors have to be addressed first or no progress can be made.
Goal setting must be mutually agreed on. The goals should be described concretely and with measurable outcomes. The therapist is trying to teach goal-oriented active problem-solving skills focused on concrete, specific patient problems. Other names for CBT have included goal setting, problem solving, self-statement modification, social perception skills training, self-control training, and cognitive restructuring. Over time, CBT can help the teen to recognize themes that identify specific maladaptive automatic thoughts.
In clinical practice, evaluation of the existing knowledge and beliefs of the individual are determined, appropriate interventions are developed to educate and motivate, and the resulting behavior changes are appraised.
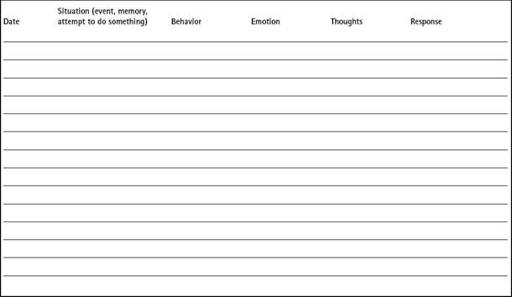
For CBT, a “thoughts log” like that shown in
Table 14-1
could be used to help the teen change his or her thinking.
Medications
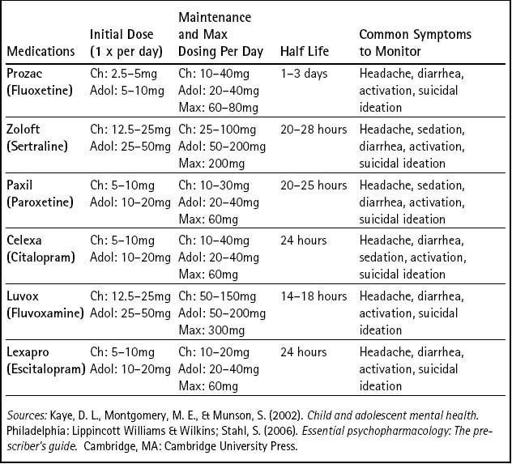
Often psychotherapy is used first for mild cases of depression. Medications may be warranted if this is not effective, or if the depression is more severe. Selective serotonin reuptake inhibitors (SSRIs) are considered the first-line treatment for depression. Food and Drug Administration (FDA) approved indications for pediatric depression controlled trials support the use of fluoxetine (Prozac), paroxetine (Paxil), and citalopram (Celexa) for children and adolescents with depression. Open trials also support the use of Prozac, sertraline (Zoloft), Paxil, Celexa, and fluvoxamine (Luvox). With respect to dosing of these medications, the rule of thumb is to “start low and go slow.” Dosing can be increased every 5–7 days to target dose and then should be held for 4–6 weeks before further dose increases.
Table 14-2
shows dosing guidelines. Medications are typically given on a QD (daily) schedule. The primary care provider may be asked by the
mental health specialist to prescribe psychotropic medications if that person does not have prescriptive authority. Even if not prescribing, the primary care provider needs to know which medications are being prescribed and provide surveillance related to safety and effectiveness.
Table 14–1 Thoughts Log
When prescribing, it is important to educate patients about side effects because this seems to help with treatment adherence. Common side effects of SSRIs include agitation or restlessness, apathy or amotivation syndrome, gastrointestinal upset or diarrhea, headaches, insomnia, and sexual side effects (Kaye et al., 2002).
Serotonin syndrome is a serious and possibly fatal syndrome that occurs when serotonin has been overstimulated. Symptoms include diarrhea, restlessness, extreme agitation, hyperreflexia, and autonomic instability with possible rapid fluctuations in vital signs, myoclonus, seizures, hyperthermia, uncontrollable shivering and rigidity, delirium, coma, status epilepticus, cardiovascular collapse, and death. Treatment includes removing the offending agent and referral to the hospital for care (Sadock & Sadock, 2007).
Table 14–2 Dosing Table for SSRIs
SSRIs and Side Effects
If intolerable side effects emerge or a maximal dosage is reached without improvement after 8–12 weeks, then an alternative SSRI should be cross-tapered and substituted. If a second SSRI trial is unsuccessful, then atypical antidepressants (bupropion, venlafaxine, mirtazapine, and duloxetine) can be tried, although it is important to note that fewer data are available on these agents. Bupropion (Wellbutrin) has stimulant-like properties and has been helpful in some adolescents with symptoms of depression and ADHD. It has been associated with increased risk of seizures and should not be used in patients with a history of substance abuse or eating disorders because it is contraindicated in these cases. Venlafaxine (Effexor) has also been shown to help symptoms of depression and anxiety in adolescents. It can cause blood pressure elevations, and 5–7% of patients on it must be monitored for these changes. Mirtazapine (Remeron) has not been used widely in adolescents. It is highly sedating and, rarely, is associated with agranulocytosis. Duloxetine (Cymbalta) also has not been widely used for adolescents, but is available. Adult data show gastrointestinal side effects. Tricyclic antidepressants are not currently supported as first-line agents for treating juvenile depression. Studies have shown that they have a narrow margin for safety and lack of benefit (Kaye et al., 2002; Sadock & Sadock, 2007).
When adolescents are taking antidepressants, the healthcare provider needs to be vigilant for signs of mania, including increased activity, irritability, aggression, euphoria, giddiness, and decreased need for sleep. If these symptoms are present the antidepressant needs to be discontinued. This can occur with use of any of the antidepressants in adolescents predisposed to bipolar disorder (Sadock & Sadock, 2007). Suicide ideation can also occur.
Both adolescents and their families need to be reminded that antidepressants often take 2–4 weeks to alleviate symptoms. The medication should be continued for 6–12 months once symptoms improve. Adolescents should be symptom-free for at least 3 months before considering tapering off of medication. Antidepressants need to be slowly tapered. This will prevent withdrawal symptoms and allow for rapid retitration if depressive symptoms reoccur (Sadock & Sadock, 2007).
In Tom’s case, it would be appropriate to start Prozac 10 mg 1 tablet PO in the morning and refer him to a therapist for CBT. It would be important to have him return weekly for 2 to 4 weeks for follow-up to report on how he is feeling and to assess for suicidal ideation.
What will you do to educate him and his mother about depression and the management of his symptoms?
The following are points you include when educating Tom about depression and it’s management:
Explain the diagnosis and its pathophysiology, its chronic nature, and the need for medications and therapy to stabilize the depressed mood.
Explain the use of the antidepressant prescribed, including efficacy and side effects. Reassure them that the medication may not result in improvement for 4–6 weeks and that the improvement may seem subtle. Often parents and teachers will notice the benefit before the teen may feel it.
Discuss monitoring for suicidal ideation and that it is important for Tom to tell his parents if he has these feelings. Tom or his parents should call you immediately so it can be determined if he might need to be hospitalized at that point.

