Pediatric Primary Care Case Studies (61 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

• Has the child been in contact with pets, especially cats? (looks for toxoplasmosis)
• Has there been any recent travel? (exposure to different infectious agents not seen in the United States)
• Is there any history of sexual assault? (possible HIV exposure)
• Does the child have a history of allergic rhinitis? (allergies)
• Has the family seen any other providers regarding this illness? (integrative medicine approach)
No one has been ill in the household or among the child’s close friends. The child is not taking any medications for health and has not been to any other provider. The child is exposed to the daycare children in the after-school program or in her gymnastics class, where the children all use the same equipment. There is no known exposure to cats or other pets. The child has no allergies and has not been sexually assaulted.
What information do you want to collect in your physical examination?
Physical Examination:
Height, weight, blood pressure, and body mass index are all on the 50th percentile for this Tanner 1 female who has not had any weight loss. The physical examination is remarkable for +3 erythematous tonsils without exudate. There are palatal petechiae on the soft palate. The anterior cervical chain is mildly tender and nodes range in size from 2–2.5 cm. The tonsillar nodes are 2 cm. The nodes are not fixed or mattered. On the right side, there is a 3 cm node on the posterior chain with a few nodes that are less than 1 cm around it. These nodes are not fixed but are tender to touch. There is no axillary, epitrochlear, inguinal, or popliteal nodes. The chest is clear and the heart sounds are normal without murmurs. There is no hepatosplenomegaly or abdominal masses present. The external genitalia is without redness, and the hymenal ring is smooth and without increased redness on gross inspection. The skin is clear without rash or petechiae.
Making the Diagnosis
The history and physical examination are consistent with IM. The family is anxious for laboratory confirmation of the diagnosis.
What initial laboratory diagnostic tests need to be ordered?
Laboratory tests are ordered to confirm a suspected diagnosis. Before ordering laboratory tests, consider the following points:
• What is the expense of the test?
• If the patient had no insurance, would you order the test?
• Which test has the lowest cost and will best help you determine the diagnosis?
• Do you know how to interpret the test including sensitivity, specificity, and predictive value for the child’s age?
• How will the lab test help you in developing a plan of care for the patient?
• Will the test satisfy the family’s concerns and need for further testing?
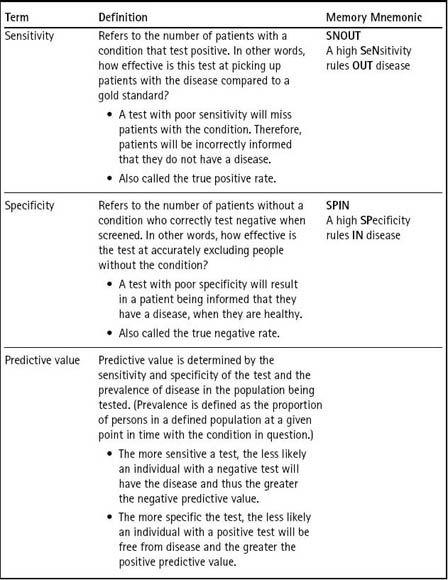
If the wrong test is ordered, the diagnosis will be delayed. In order to choose a diagnostic test, it is important to consider the test’s specificity and sensitivity and to recognize that these can vary with the age of the child. These concepts are explained further in
Table 16-2
. In trying to determine which test to order, sensitivity, specificity, prevalence, predictive value, and cost must be considered. The main reason to investigate with serology is to confirm the cause of symptoms.
An initial diagnostic strategy would be to do a heterophile antibody test (Bell & Fortune, 2006; Smellie et al., 2007) and a complete blood count (CBC) to look for lymphocytosis and atypical lymphocytes. Each is discussed here.
The Paul Bunnell heterophile antibody is a group of IgM class immunoglobulins that are present when someone has an acute EBV infection. The structurally similar epitropes in the nonhuman RBC (sheep, horse, pig) in the test react
with the Paul Bunnell heterophile antibody, resulting in red cell agglutination. In adolescents and adults, up to 85% who have clinical IM have detectable Paul Bunnell heterophile antibodies. The antibodies develop during the first week and peak between the second and fifth week of illness (Hurt & Tammaro, 2007). The range of sensitivity for this test is between 71% and 90% (Linderholm, Boman, Juto, & Linde, 1994); however, the results of heterophile antibody testing is lower in children under 12, ranging from 25–50% (Bruu et al., 2000). During the first week of illness, there is a 25% false negative rate (Ebell, 2004).
Table 16–2 Understanding Sensitivity and Specificity
Rapid Monospot tests are enzyme-linked immunosorbent assay (ELISA) techniques to look for EBV virus infection. Rapid tests may be available in the office depending on insurance reimbursement. Thus, a positive heterophile antibody test or Monospot test indicates that the child has EBV IM; however, a negative Monospot in this girl may mean that the test was done too early in the course of the illness, the child will not react because she is young, or the child has a heterophile-negative mononucleosis-like illness caused by CMV, HIV, or toxoplasmosis. Thus for younger children, this test may not be as helpful.
The CBC during the first week of illness may not show lymphocytosis or increased atypical lymphocytes. As the number of atypical lymphocytes increase, the specificity of the test increases. Remembering the mnemonic
SPIN
helps: A high
SP
ecificity rules
IN
disease. When the number of atypical lymphocytes is greater than 10%, the sensitivity is 75% and the specificity is 92%. When it goes up to greater than 40%, the sensitivity is 25% and the specificity is 100% (Bell & Fortune, 2006). (See
Table 16-2
.) Thus, the higher the atypical lymphocyte count, the greater the likelihood of IM.
You make a presumptive diagnosis of IM based on Maya’s history and clinical findings and begin your discussion with her mother regarding the management plan and laboratory testing that you will do to confirm your IM diagnosis. The reason that a presumptive diagnosis is made at this time is based on the fact that Maya’s course of illness is six days in duration and the Monospot test can come back negative during the early course of illness, thus, giving a false negative result.
Management
How do you plan to treat the child’s infectious mononucleosis?
Therapeutic plan: What will you do therapeutically?
The plan is symptom-based and customized to the child’s presentation and the family’s desires. The goals are to:
• Control fever
• Keep the child hydrated
• Provide enough calories to prevent weight loss
• Allow adequate rest opportunities
• Treat secondary bacterial infections
• Provide opportunities to do school work by coordinating with the school for homework and, if the illness continues, a home tutor
• Avoid splenic rupture by limiting contact play or sports
• Determine the cause of the IM
Treatment Options
Treatment for EBV and CMV IM is symptom based. The use of antipyretics to control fever and keeping the child in light clothing to allow for heat dissipation is important. Appropriate foods and liquids that avoid irritating the throat need to be suggested with cultural sensitivity. Discussing what foods Maya eats and choosing which ones might be tolerated is helpful to the family. Liquids that would be tolerated are selected with input from the family. Because group A streptococcus is a secondary infection for patients with IM, the family is encouraged to finish the Omnicef. At this point, the mother is given a note for the school for school work and the need for a home tutor.
Each school system determines the length of time that a child must be out before a home tutor is allowed during a prolonged illness; however, giving the school notice that an illness is likely to be prolonged can help them plan and get the tutor in the house sooner.
There is no medication to treat EBV or CMV IM. The use of acyclovir has not proved to shorten the course of illness (Torre & Tambini, 1999). A recent Cochrane review noted there was insufficient evidence to recommend steroid treatment for symptom control in IM (Candy & Hotopf, 2008). There was also a lack of research on the long-term side effects in patients treated with steroids, including lymphoproliferative disorders (Candy & Hotopf).
Educational plan: What will you do to educate Maya and her family about IM?

