Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (4 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
11.82Mb size Format: txt, pdf, ePub
• Intracranial bleed (“cerebral T waves,” usually w/ ↑ QT)
• Normal variant in children (V
1
–V
4
) and leads in which QRS complex predominantly
Low voltage
• QRS amplitude (R + S) <5 mm in all limb leads & <10 mm in all precordial leads
• Etiologies: COPD (precordial leads only), pericardial effusion, myxedema, obesity, pleural effusion, restrictive or infiltrative CMP, diffuse CAD
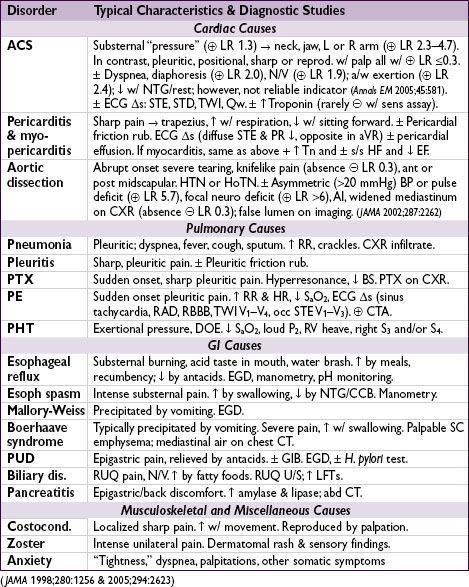
CHEST PAIN
Initial approach
•
Focused history
: quality & severity of pain; location & radiation; provoking & palliating factors; intensity at onset; duration, frequency & pattern; setting in which it occurred; associated sx; cardiac hx and risk factors
•
Targeted exam
: VS (including BP in both arms), cardiac gallops, murmurs or rubs; signs of vascular disease (carotid or femoral bruits, ↓ pulses), signs of heart failure; lung & abdominal exam; chest wall exam for reproducibility of pain
•
12-lead ECG
: obtain w/in 10 min; c/w priors & obtain serial ECGs; consider posterior leads (V
7
–V
9
) to reveal posterior MI if hx c/w ACS but ECG unrevealing or ST ↓ V
1
–V
4
•
Cardiac biomarkers (Tn
±
CK-MB)
: ✓ Tn at baseline & 3–6 h after sx onset
troponin
: >95% Se, 90% Sp; level >99th %ile w/ rise & fall in approp. setting is dx of MI detectable 1–6 h after injury, peaks 24 h, may remain elevated for 7–10 d in STEMI
high-sens. Tn
: 98% Se, 90% Sp w/in 3 h of admit, 90% Se w/in 1 h (
JAMA
2011;306:2684)
Causes for ↑ Tn other than ACS (= “type 1 MI”): (1) Supply-demand mismatch not due to Δ in CAD (= “type 2 MI”; eg, ↑↑ HR, shock, HTN crisis, spasm, HCM, severe AS), (2) non-ischemic injury (myocarditis/toxic CMP, cardiac contusion) or (3) multifactorial (PE, sepsis, severe HF, renal failure, Takotsubo, infilt dis.) (
Circ
2012;126:2020)
CK-MB
: less Se & Sp (skel. muscle, tongue, diaphragm, intestine, uterus, prostate), useful for dx of post-PCI/CABG MI or MI if Tn already elevated
•
CXR
; other imaging (echo, PE CTA, etc.) as indicated based on H&P and initial testing
• If low prob of ACS (eg,ECG & Tn) & stable → noninvasive fxnal or imaging test
• Coronary CT angio (CCTA): NPV 98% for signif CAD, but PPV 35% for ACS; helpful to r/o CAD if low-intermed prob of ACS. CCTA vs. noninv. fxnal test for ischemia → ↓ time to dx & LOS, but ↑ prob of cath/PCI, contrast exposure & ↑ radiation (
NEJM
2012;366:1393 & 367:299;
JACC
2013;61:880). “Triple r/o” CT angiogram for CAD, PE, AoD.
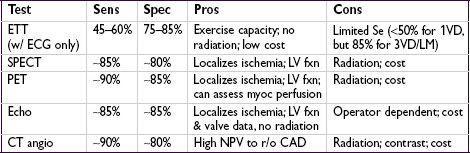
NONINVASIVE EVALUATION OF CAD
Stress testing (
Circ
2007;115:1464;
JACC
2012;60:1828)
•
Indications
: dx CAD, evaluate Δ in clinical status in Pt w/ known CAD, risk stratify s/p ACS, evaluate exercise tolerance, localize ischemia (imaging required) •
Contraindications
(
Circ
2002;106:1883; & 2012;126:2465)
Absolute
: AMI w/in 48 h, high-risk UA, acute PE, severe sx AS, uncontrolled HF, uncontrolled arrhythmias, myopericarditis, acute aortic dissection
Relative
: left main CAD, mod valvular stenosis, severe HTN, HCMP, high-degree AVB, severe electrolyte abnl
•
Exercise
: standard Bruce (↑ speed & incline q3min), modified Bruce (begins w/o treadmill incline), submax (if <3 wk post-MI) or sx-limited; hold nitrates/βB/CCB/ranolazine if trying to dx CAD, but give when assessing if Pt ischemic on meds •
Pharmacologic
: if unable to exer., low exer. tol, or recent MI. Se & Spexercise. Preferred if LBBB (requires imaging since ECG not interpretable).
Coronary vasodilators
(will reveal CAD, but
not
tell you if Pt
ischemic
): regadenoson, dipyridamole or adenosine (may precipitate bradycardia and bronchospasm).
Chronotropes/inotropes
(more physiologic): dobutamine (may precipitate tachyarrhythmias).
•
Imaging
: used if uninterpretable ECG (paced, LBBB, resting ST ↓ >1 mm, dig., LVH, WPW), after indeterminate ECG test, pharmacologic tests, or localization of ischemia
SPECT
(eg,
99m
Tc-sestamibi),
PET
(rubidium-82; usually w/ pharm test),
echo
,
MRI
Test results
•
HR
(must achieve ≥85% of max pred HR [220-age] for
exer
. test to be dx),
BP
response, peak
double product
(HR × BP; nl >20k), HR recovery (HR
peak
– HR
1
min later
; nl >12) •
Max exercise capacity
achieved (METS or min) • Occurrence of
symptoms
(at what level of exertion and similarity to presenting sx) •
ECG
Δ
s
:
downsloping
or
horizontal
ST ↓ (≥1 mm) 60–80 ms after QRS predictive of CAD (but does
not
localize ischemic territory); however, STE highly predictive & localizes • Duke treadmill score = exercise min – (5 × max ST dev) – (4 × angina index) [0 none, 1 nonlimiting, 2 limiting]; score ≥5 → <1% 1-y mort; –10 to + 4 → 2–3%; ≤ –11 → ≥5%
•
Imaging
: radionuclide defects or echocardiographic regional wall motion abnormalities
reversible defect = ischemia; fixed defect = infarct; transient isch dilation = severe CAD
false: breast → ant “defect” and diaphragm → inf “defect”
falsemay be seen if balanced (eg, 3VD) ischemia (global ↓ perfusion w/o regional Δs)
High-risk test results (PPV ~50% for LM or 3VD, ∴ consider coronary angio)
• ECG: ST ↓ ≥2 mm
or
≥1 mm in stage 1
or
in ≥5 leads
or
≥5 min in recovery; ST ↑; VT
• Physiologic: ↓ or fail to ↑ BP, <4 METS, angina during exercise, Duke score ≤ –11; ↓ EF
Other books
The Storyteller of Marrakesh by Joydeep Roy-Bhattacharya
The Second Book of General Ignorance by John Lloyd, John Mitchinson
Bette and Joan The Divine Feud by Considine, Shaun
Dangerous Waters by Juliet E. McKenna
Unexpected Gifts by S. R. Mallery
Because It Is My Blood by Zevin, Gabrielle
1920 by Eric Burns
Arrows of Fury: Empire Volume Two by Riches, Anthony
Strip Tease by Carl Hiaasen
The Accidental Pope by Ray Flynn