Vaccinated (6 page)
Authors: Paul A. Offit

Although many cancer researchers working in the 1910s through the 1940s ignored Rous's findings, evidence continued to mount in favor of cancer-causing viruses. In the early 1930s Richard Shope, a veterinarian from Iowa, found that viruses caused giant warts on wild rabbits in the southwestern United States. (Although many consider them to be mythical creatures, jackalopesâjackrabbits with antelope hornsâmight be rabbits infected with Shope's wart-causing virus.) A few years later, researchers found a virus that caused tumors in the mammary glands of mice. But it wasn't until the 1950s, when Ludwik Gross, a Polish refugee, found a virus that caused leukemia in mice, that cancer-causing viruses came out of the cabinet and into the mainstream of virus research. Ten years later William Jarrett, working at the University of Glasgow in Scotland, found another virus that spread easily from one cat to another, causing leukemia. Not only did viruses cause cancer, but some cancer-causing viruses were also contagious.
In 1966, more than fifty years after he had examined the farmer's dead chicken, Peyton Rous won the Nobel Prize in medicine for “the discovery of tumor-inducing viruses.” Rous received the prize, which cannot be awarded posthumously, when he was eighty-six years old.
Â
T
ODAY WE KNOW THAT SOME OF THE VIRUSES THAT CAUSE CANCER
belong to the family of retroviruses, the most famous of which is human immunodeficiency virus (HIV), the virus that causes AIDS. When John Enders handed a vial of measles vaccine to Maurice Hilleman, it was loaded with a retrovirus that caused leukemia in chickens. Although they didn't know it, chicken leukemia virus had contaminated the eggs that the Enders team had used to make their vaccine.
At the time Hilleman wanted to make his measles vaccine, chicken leukemia virusâsimilar to the one that had infected Peyton Rous's chickenâinfected about 20 percent of all chickens in the United States. The virus infected the liver, causing liver cancer; the kidneys, causing kidney cancer; ligaments, tendons, and skin, causing soft-tissue cancers; and cells of the immune system, causing leukemia and lymphoma. About 80 percent of chickens infected with chicken leukemia virus got leukemia. The virus was a tremendous headache for farmers, causing $200 million in lost revenue every year. Worse, in the early 1960s, researchers didn't know whether viruses that caused cancer in chickens could cause cancer in people. But they did know that animal retroviruses like chicken leukemia virus were capable of causing human cells in a test tube to become cancerous. “I wasn't going to license a vaccine with this virus in it,” said Hilleman. “That would be the most unethical thing.” Despite pressure from people such as Joe Smadel, director of the federal agency that licensed vaccines, to bring Enders's vaccine to market quickly, Hilleman refused to ignore the remote possibility that chicken leukemia virus could cause cancer in people. “Here was a vaccine that had been grown in cell culture, still highly virulent, and grown in cells that were loaded with leukemia virus,” recalled Hilleman. “And I'd be damned if I was going to vaccinate all of these kids with [a virus causing] leukemia. I wouldn't do it. The government wanted to move forward because kids were dying [of measles]. When I told Smadel that we weren't going to bring out the [vaccine] with leukemia [virus] in it, he had a temper tantrum.”
Although chicken leukemia virus was common, no one had found a way to detect it. And because contaminated eggs appeared perfectly normal, researchers couldn't tell which eggs were infected and which weren't. Hilleman was stuck. Fortunately, in 1961 a virologist at the University of California at Berkeley, Harry Rubin, found a way to detect chicken leukemia virus in the laboratory. “The Rubin test changed everything,” recalled Hilleman. With Rubin's test now in hand, Hilleman could use eggs and chick embryos that didn't contain chicken leukemia virus to make his vaccine. First, Hilleman tried to breed his own flock of leukemia-virusâfree chickens. But Merck was a company better suited to making drugs than to breeding chickens. So Hilleman turned to his friend Wendell Stanley for help. Stanley, who had won the Nobel Prize in medicine in 1946 for his work determining the structure of virus particles, directed Hilleman to a small farm in the Niles section of Fremont, California, Kimber Farms, where researchers had successfully bred a flock of leukemia-virusâfree chickens. Hilleman found this hard to believeâhe knew how much trouble he was having breeding them at Merckâbut he was willing to give it a shot. So he got on a plane and flew to San Francisco. Then he drove forty miles to Fremont.
Â
N
ILES WAS SMALL, CENTERED ON AN OLD FLOUR MILL, A
S
OUTHERN
Pacific Railroad switching yard, some fruit packing plants, and a company that excavated sand and gravel.
Kimber Farms, part of the poultry-genetics mania that began in the early 1900s, was founded in the early 1930s by John Kimber, whose father was an Episcopal minister and mother a professional musician. Kimber was enormously successful, proving that the quality and size of an egg, the thickness of the shell, and the number of eggs produced could all be controlled by scientific breeding. He developed disease-free eggs, disease-resistant chickens, and hens that could lay two hundred and fifty eggs per yearâaccomplishments communicated to local farmers through his newsletter,
Kimberchik News
. But the notion of genetically breeding animals for food didn't sit well with critics, who saw Kimber's breeding operation as heartless and cruel. “Efficient, white-gowned workers in the antiseptic laboratories of Kimber Farms had little time for sentiment,” recalled Page Smith and Charles Daniel, authors of
The Chicken Book
. “To them the baby chickens, half of whom were killed at birth and incinerated or fed to the hogs, hatched by the millions in their enormous incubators, [were] seen primarily as items on an assembly line. The fact that they were alive was, it seems fair to suggest, incidental.”
To make chickens and eggs free of leukemia virus, Kimber scientists took eggs from hens that weren't infected with the virus, dipped them in organic iodine, and carefully put them into a sterile incubator. Male and female chickens born from these eggs made more chickens. Within a single generation, researchers at Kimber had bred chickens that were free of chicken leukemia virus. But it wasn't easy. The chickens were housed two hundred feet upwind from the nearest poultry house and screened to prevent contact with flies and rodents. Furthermore, caretakers had to put on protective clothing and shoes and step in a foot-pan containing disinfectant before entering the building. At the time, Hilleman didn't have the facilities or expertise at Merck to duplicate these procedures.
When Hilleman arrived at Kimber Farms, he walked into the main office and asked to speak to the principal investigator, Walter Hughes. He asked Hughes if he could buy some of his leukemia-free chickens. “That's our research flock,” said Hughes. “I can't sell you those chickens.” Hilleman considered his next move. “Do you have a boss?” he asked. Hughes escorted Hilleman into the office of the director of poultry research, W. F. Lamoreux. The result was the same. Lamoreux didn't want to sell his chickens. Hilleman tried harder: “One year from now there are going to be a lot of dead kids from measles, and you can do something to stop it.” Lamereux wasn't moved. “We're not selling our chickens,” he said. As Hilleman was leaving the office, he stopped, turned around, and tried one more time. Recognizing a familiar accent, he asked Lamoreux where he was from. “Helena,” said Lamoreux. “Miles City,” replied Hilleman, extending his hand. “Take them all,” said Lamoreux, smiling broadly. “One buck apiece.”
The first measles vaccine required a virologist and a chicken breeder. If both hadn't been born and raised in Montana, the road to a lifesaving vaccine might have been much longer.
Â
H
ILLEMAN LATER SET UP HIS OWN FLOCK OF LEUKEMIA-VIRUSâFREE
chickens on the Merck grounds, and between 1963 and 1968 he made millions of doses of Enders's measles vaccine. The vaccine worked. Despite the burden of its having to be given with gamma globulin, it decreased the incidence of measles in the United States. But Hilleman wasn't the only researcher, and Merck wasn't the only company to make measles vaccine. Two other pharmaceutical companies introduced their own vaccines. One, a vaccine made in dog kidneys by a veterinary vaccine maker, was on the market for only three weeks. “That vaccine was more dangerous than measles,” recalled Hilleman. The other vaccine, made by killing natural measles virus with formaldehyde, was given to about a million American children before researchers found that immunity was dangerously short lived. Public health officials withdrew the killed measles vaccine after it had been sold for only four years.

For his work on the measles vaccine, Maurice Hilleman was interviewed in 1963 by Charles Collingwood of CBS. The segment was titled “The Taming of a Virus.”
Despite the success of Hilleman's measles vaccine, the need to give it with gamma globulin made it cumbersome to use. To solve the problem, Hilleman took Enders's measles vaccine and passed it forty more times through chick embryo cells. He called this new strain the Moraten strain, for
Mor
e
Attenuated En
ders. Merck first distributed the Moraten strain in 1968. Since then, it has been the only measles vaccine used in the United States. Between 1968 and 2006, hundreds of millions of doses have been given. As a result, the number of people infected every year with measles in the United States has decreased from four million to fewer than fifty. Worldwide, the number of people killed by measles every year has decreased from eight million to about five hundred thousand. Measles vaccines save more than seven million lives a year. And the descendants of Kimber Farms's original flock of chickens, still maintained on the grounds of Merck, are used to make vaccines today.
What would have happened if Maurice Hilleman had made his measles vaccine using eggs contaminated with chicken leukemia virus? Would the vaccine have caused leukemia or other cancers? The answer came in 1972, ten years after Hilleman had licensed his first measles vaccine. Researchers studied about three thousand veterans of the Second World War who had died of cancer to see whether they were likely to have received a yellow fever vaccine made in eggs contaminated with chicken leukemia virus. The answer was no. Although chicken leukemia virus caused cancer in chickens, it didn't cause cancer in humans. But when Maurice Hilleman made his measles vaccines, he didn't know that. “I just couldn't take that chance,” he recalled.
5
Coughs, Colds, Cancers, and Chickens
“This blender is going to revolutionize American drinks.”
F
RED
W
ARING
B
etween 1944, when he left the University of Chicago to work at E. R. Squibb, and 1968, when he made his own measles vaccine at Merck, Maurice Hilleman made or tried to make several unusual vaccines.
One prevented cancer.
Hilleman's vaccines to prevent measles, mumps, and pandemic influenza all had one thing in common: they were made in chickens. “Chickens were my best friend,” he said. “I could hypnotize them. All you had to do was lay them on their side and let them stare at a white feather. They were transfixed by that feather. They helped me so much. Maybe I could do something for them.” When Hilleman finally paid his debt to chickens, he also fulfilled a promise that was made, but never kept, by Herbert Hoover.
During the 1928 campaign for the presidency of the United States, newspaper advertisements by the Republican National Committee proclaimed that Warren Harding and Calvin Coolidge had “reduced [work] hours and increased earning capacity, silenced discontent, put the proverbial âchicken in every pot,' and a car in every backyard, to boot.” The advertisement stressed that a vote for Herbert Hoover was a vote for continued prosperity. The promise of a chicken in every pot was attractive. Chickens, like turkeys today, were expensive, served only as a delicacy for special occasions. But Herbert Hoover, who presided over the stock market crash of 1929 and the beginning of the Great Depression of the 1930s, never kept the promise.
Hilleman remembered a strange disease that had affected chickens on his family's farm when he was a child: “Every year we had chickens that would die or become ill from an unknown cause.” Some chickens destined for the Hillemans' dinner table were thin and weak or had ghastly, rock-hard tumors under their skin or in their organs. “[Aunt Edith] would have a chicken killed now and then. When she saw a chicken that had lumps on the skin or had any tumors, she would say âWe can't eat that.'” Years later, the mysterious ailment had a name: Marek's disease. By the early 1960s, researchers found that Marek's disease was caused by a herpesvirus.
Marek's disease wasn't a problem only on the Hilleman farm. It was a problem on many farms, affecting 20 percent of all chickens produced in the United States. The disease attacked the nerves of the legs, causing paralysis; chickens died because they couldn't get food and water or because they were trampled by other birds. Farmers called it “range paralysis,” referring to infected chickens as being “down in the leg.” The virus also caused cancer of the skin, ovaries, liver, kidneys, heart, and spleen, killing one third of its victims. There was no treatment. Farmers simply culled infected chickens from the flock and destroyed them.
Marek's disease was also highly contagious. The virus hid in the fine, light dandruff that filled the air of the chicken coop. “We had these chickens dying all the time with range paralysis,” recalled Hilleman. “[In the chicken coop] there were these great festoons of chicken dandruff. We had a wire hanging down from the ceiling, and it would be just like a hive of bees swarming.” Because of its surface charge, the dandruff would cling to the wires. “Electrostatically, you would have one or two gallons of chicken dandruff hanging on there.” The light spray of dandruff hung in the air for months, easily spreading from coop to coop and farm to farm.
Hilleman had seen Marek's disease and remembered it. When Ben Burmester, a veterinary researcher in Michigan, found that a herpesvirus similar to Marek's virus also caused disease in turkeys and quail, Hilleman saw his opening. “One day I get a call from Burmester from the East Lansing Regional Poultry Center,” recalled Hilleman. “[He] said, âMaurice, we've isolated a virus here from turkeys, and when we vaccinate chickens, they become resistant to Marek's disease.' I said âBen, I'll be out tomorrow.' I asked him, âWhat is your interest?' And [Ben] told me, âI just made an observation, I can't do anything with it.'”
Hilleman took Burmester's turkey herpesvirus, grew it in the laboratory, injected it into one-day-old chicks, and found that they were protected from Marek's disease. But before he could distribute his Marek's vaccine, Hilleman had one more obstacle. He had to convince Merck's board of directors to get into the chicken vaccine business. Max Tishler, Hilleman's boss and the director of research at Merck, set up a meeting with the board. Tishler wasn't interested in making products for animals and was certain that the board would agree. “I got hell [from Tishler] for developing the product,” recalls Hilleman. “I was asked to go to the board of directors, and the directors said, âThat's wonderful; go ahead.' Max came running after me after the meeting and said, âWhy did you do that?' I said âYou were the one who told me to go to the meeting.' And [Tishler] said, âYeah, but I didn't want you to succeed. We're not in the chicken business.' [Marek's disease] vaccine was such a drain on our laboratory. But it was the world's first cancer vaccine.” Merck, like it or not, was now selling products made for chickens. Soon it would be selling the chickens too.
Chicken farmers are in the business of converting carbohydrate (grain) into protein (meat). “There are two kinds of chicken breeders in this world,” recalled Hilleman. “There are those who breed chickens to get maximum egg production, and those who breed for maximum meat production. They all, with the exception of one company, would breed for resistance to Marek's disease.” The one company was Hubbard Farms of Walpole, New Hampshire.
In 1921 Oliver Hubbard, one of the first students to graduate from the University of New Hampshire with a degree in poultry farming, founded Hubbard Farms. By the early 1930s, Hubbard had developed the New Hampshire chicken, a breed unrivaled for egg and meat production. But there was one problem. The New Hampshire chicken was more susceptible to Marek's disease than any other breed. “Hubbard Farm chickens were by far the most productive means of converting carbohydrate to protein than any other chicken in the world,” remembered Hilleman. “But if you got Marek's into the flock, you were done.” Hilleman saw an opportunity for Merck. “Merck was out for an acquisition, and it was obvious what to do. We'll buy Hubbard! [We'll combine] these efficient carbohydrate-to-protein chickens with the vaccine that compensated for their genetic susceptibility to Marek's disease.”
In 1974, Merck bought Hubbard Farms for $70 million. Hilleman's vaccine, the first to prevent cancer in any species, revolutionized the poultry business. Excess production caused the price of chickens to drop from $2 per broiler to forty cents and of eggs from fifty cents per dozen to five cents. Soon everyone could afford chickens, and for a while, Merck, one of the more conservative pharmaceutical companies in the United States, was the biggest chicken and egg producer in the world.
Â
W
ITH HIS
M
AREK
'
S VACCINE,
M
AURICE
H
ILLEMAN BECAME THE FIRST
person to make a vaccine to prevent cancer. He was also the first person to purify, characterize, and produce a drug that is now used to treat certain cancers in people.
In the early 1900s Alexander Fleming, a Scottish biologist working in London, returned from a vacation to find something unusual in his laboratory. Fleming worked with
Staphylococcus aureus
, a bacterium commonly found on the skin and in the environment. He grew the bacteria in laboratory plates, where it formed small golden-yellow colonies (in Latin
aureus
means “gold”). When Fleming returned to the laboratory after several weeks he found, much to his dismay, that the plates had been overrun with mold: fluffy green mold. But he also noticed something else. Although many colonies of bacteria were present throughout the dish, he didn't see any in the areas immediately surrounding the mold. Fleming reasoned that a substance produced by the mold was killing the bacteria. Because the name of the mold was
Penicillium notatum
, Fleming called the substance penicillin. In 1929 Fleming published a paper titled “On the Antimicrobial Action of Cultures of a Penicillium with Special Reference to Their Use in the Isolation of B. Influenzae.” Fleming's first description of penicillin is regarded as one of the most important medical papers ever written.
For the next six years Alexander Fleming worked fitfully on his new antibiotic. But Fleming was a biologist, not a chemist; he never successfully purified penicillin. In 1935, six years after publishing his discovery, he gave up. Several years later, at the start of the Second World War, a team of researchers at Oxford University headed by Howard Florey picked up where Fleming had left off. They purified penicillin, described its physical and chemical properties, studied its effects in animals and humans, and showed how to mass-produce it, just in time to save the lives of tens of thousands of Allied soldiers.
Ten years after abandoning his research on penicillin, Alexander Fleming won the Nobel Prize in medicine “for the discovery of penicillin and its curative effect in various infectious diseases.” Although our understanding of what penicillin is, how it works, and how it can be used to save lives couldn't have happened without Howard Florey, few know his name. When people think of penicillin, they think of Alexander Fleming. The story of Fleming and Florey would be repeated with the discovery of the first substance to inhibit the growth of viruses and treat cancer.
In 1957 Alick Isaacs, a Scottish virologist working on influenza virus, teamed with a Swiss biologist named Jean Lindenmann. Working in Mill Hill Laboratories just outside of London, they found, as had many researchers before them, that influenza virus destroyed cells in the membrane that surrounded chick embryos. But unlike other researchers, they found that if they first treated the chick cells with a strain of killed influenza virus, then live influenza virus didn't destroy the cells. Isaacs and Lindenmann reasoned that chick cells exposed to killed influenza virus were making a substance that inhibited the ability of influenza virus to grow. They called this interfering substance
interferon
. Isaacs thought that biologists had now described their own unique element. “It is time that biologists had a fundamental particle,” he said, “for the physicists have so many: electron, neutron, proton.” Many skeptical scientists disagreed, preferring to call Isaacs and Lindenmann's finding an “imaginon.”
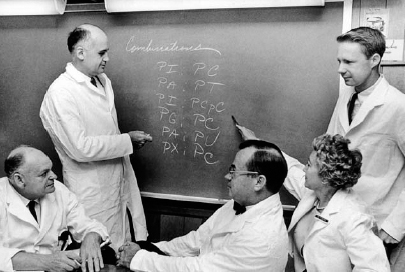
Maurice Hilleman and the interferon team at Merck, circa early 1960s.
Unfortunately, Isaacs and Lindenmann couldn't purify interferon, so they couldn't study what it was or how it worked. Hilleman, by figuring out how to mass-produce it, revolutionized the field of interferon research. Where Isaacs and Lindenmann's preparation contained seventy units of interferon per milliliter (one fifth of a teaspoon of liquid), Hilleman's contained more than two hundred thousand. Hilleman's final product was so pure that one unit of interferon activity was contained in only forty nanograms of protein (about one two-millionths of the weight of a grain of sand)âa potency to treat viruses that was, on a weight basis, actually greater than the potency of penicillin to treat bacteria.
Because he was the first to purify interferon, Hilleman was the first to detail its physical, chemical, and biological properties. He found that interferon was produced not only by cells from chick embryos but also by cells from calves, hamsters, dogs, rabbits, mice, and humans. He found that interferon inhibited the growth of many human and animal viruses, including cowpox, rabies, and yellow fever. He found that interferon not only prevented infections caused by viruses but also prevented cancers caused by viruses. “Interferon was the first antiviral agent, the grandfather of them all. It was a real good inducer of resistance,” recalled Hilleman. “We could stop [cancer-causing] viruses. We could stop nearly every god-damned virus.”
In the mid-1960s, Maurice Hilleman reasoned that interferon could be useful in treating chronic infections and cancers. And he was right. Today interferon is used in the treatment of chronic infections with hepatitis B and hepatitis C viruses, as well as cancers such as leukemia, lymphoma, and malignant melanoma.
Â
H
ILLEMAN MADE ONE OF HIS VACCINES IN A LEAKY
W
ARING BLENDER.
In 1944, when the United States was preparing to invade the Far East, the military became very concerned about a virus called Japanese encephalitis virus (JEV), one of the most common infections of the brain in the world. Transmitted by mosquitoes, JEV causes seizures, paralysis, coma, and death in one of every three of its victims; another third are left with permanent brain damage. Indeed, JEV is still a common infection in Southeast Asia. Every year the virus infects twenty thousand peopleâmostly childrenâand kills six thousand.
Because American servicemen had never been exposed to JEV, they were, like the children of Asia, highly susceptible to the disease and its consequences. Military health officials asked pharmaceutical companies to submit bids for the production of JEV vaccine. Hilleman had just taken a job at E. R. Squibb. He wanted Squibb to win the contract. While at the University of Chicago, Hilleman had found that JEV could be grown in mouse brains and killed with formaldehyde. He also knew from studies performed in Russia and Japan that formaldehyde-treated JEV could prevent disease. “We [at Squibb] put out a bid for $3 a dose and said that we could have a production facility up and running in thirty days,” he said.
