Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (176 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

TABLE 5–8. Comparison of Different Mechanisms of Jaundice
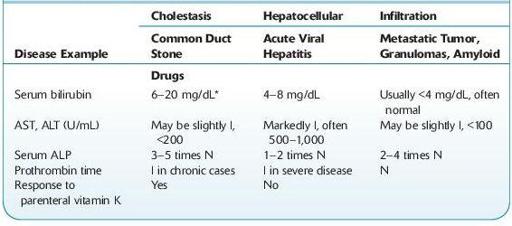
N, normal; I, increase.
*Serum bilirubin >10 mg/dL is rarely seen with common duct stone and usually indicates carcinoma. Increased serum ALP <3× normal in 15% of patients with extrahepatic biliary obstruction, especially if obstruction is incomplete or due to benign conditions. Occasionally, AST and LD are markedly increased in biliary obstruction or liver cancer.
TABLE 5–9. Comparison of Three Main Types of Liver Disease Due to Drugs
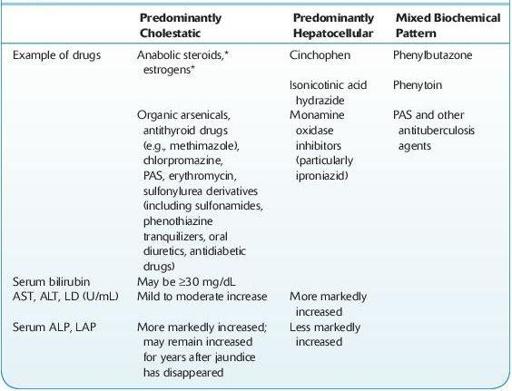
*ALP, AST, and ALT are not increased as much compared with other drugs.
INFECTIOUS DISEASE: VIRAL HEPATITIS
Definition
Five hepatitis viruses cause the majority of clinically important viral infections of the liver: HAV, HBV, HCV, HDV, and HEV. They are all RNA viruses except for HBV, which is a DNA virus. All of these viruses can cause acute hepatitis; only HBV, HCV, and HDV are able to cause chronic hepatitis infections in immunologically normal patients. Coinfection with two hepatitis viruses or hepatitis virus infection in patients with preexisting liver disease is frequently associated with greater disease severity (Table
5-10
). Other viruses or infectious agents may cause liver infection associated with systemic or localized infections. Agents include herpes viruses—like HSV, CMV, and EBV—rubella,
M. tuberculosis
, ameba, and leishmania. See the discussions for these agents in Chapter
11
.
Infectious Diseases
. A variety of hepatotoxins, autoimmune diseases, and other diseases may also cause hepatitis that is clinically similar to diseases caused by the hepatitis viruses.
TABLE 5–10. Comparison of Different Types of Viral Hepatitis
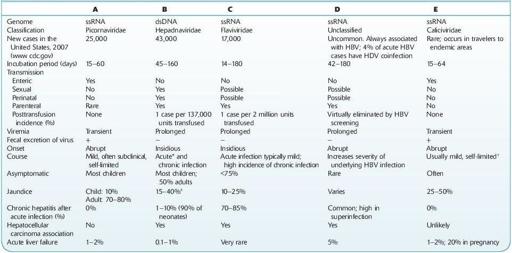
*≤20% have serum sickness-like prodroma.
† Resembles hepatitis A. Case fatality 1–2% except ≤ 20% in pregnancy; usually milder infection and biochemical abnormalities than HBV or HAV infection.
‡ A nonicteric patient is more likely to progress to chronic hepatitis. One percent of icteric cases become fulminant (<8 weeks) and 90% die within 2–4 weeks; associated with encephalopathy; renal, electrolyte, acid-base imbalances; hypoglycemia; coagulation derangements.
Viral hepatitis may be suspected in patients with nonspecific symptoms (see Prodromal Phase) or specific symptoms, like jaundice or RUQ pain (see Acute Phase). Viral hepatitis may also be considered in asymptomatic patients in whom liver function abnormality, like hyperbilirubinemia or elevated levels of AST or ALT, is detected by screening tests. For these patients, evaluation with an acute hepatitis panel is recommended; the different viral agents cannot be reliably distinguished by clinical signs and symptoms. The acute hepatitis panel includes hepatitis A IgM antibody, hepatitis B core IgM antibody, hepatitis B surface antigen, and hepatitis C antibody. Further testing, as described below, is recommended on the basis of results of the tests in the acute hepatitis panel.
Laboratory Overview
The results for acute hepatitis panel, and additional virus-specific tests, are discussed with the agents below.
Because the signs and symptoms of infection with other infectious agents and hepatotoxins may be indistinguishable from those caused by the hepatitis viruses, specific testing to rule out other causes of liver damage is recommended, based on clinical history, epidemiology, laboratory, and other relevant information.
In addition to testing for specific viral markers of infection, the patient’s hematologic, coagulation, and hepatic function should be evaluated over the course of illness.
The earliest laboratory signs of acute viral hepatitis include elevations in ALT and AST, which typically precede elevation of bilirubin levels. In acute illness, the degree of ALT elevation typically exceeds AST elevation. Peak aminotransferase levels >1,000 U/L are common. The level of aminotransferase elevation does not reliably predict the severity or prognosis of disease. Total bilirubin may increase to 5–20 mg/dL at peak. ALP is normal or mildly elevated in most cases.
CBC may show mild neutropenia with a relative lymphocytosis, often with atypical lymphocytes. Serum globulins are normal or mildly elevated. In severe liver disease, synthesis of albumin and coagulation factors may be compromised, resulting in increased PT.
