Whole-Food Guide for Breast Cancer Survivors (18 page)
Read Whole-Food Guide for Breast Cancer Survivors Online
Authors: Edward Bauman

As you can see, anything that compromises digestion can have a profound effect on the health and equilibrium of your entire body. Let’s take a closer look at some ways to lose the digestive blahs and keep your digestion dancing, thus maximizing your ability to keep breast cancer at bay.
Assessing Your General Digestive Status
Indications of poor digestion manifest in various ways, sometimes as symptoms that seemingly have nothing to do with your gut. Here are just
some
of the signs to pay attention to (Lipski 2005):
- Abdominal pain
- Bloating
- Constipation
- Diarrhea
- Rectal itching
- Undigested food particles in stool
- Poor immunity
- Recurrent vaginal infections
- Iron deficiency
- Asthma
- Joint pain or arthritis
- Skin conditions, such as eczema, psoriasis, acne, or rosacea
- Fuzzy thinking and poor memory
- Chronic autoimmune disorders
Lab Assessments
To get a clearer picture of
exactly
what’s going on in your gut, you can get a stool panel analysis by a lab such as DiagnosTechs or Metametrix. Simply order this panel through a doctor, nutritionist, or other qualified health care provider who is familiar with their use. This test offers unique insights into what is happening in your gut from a
functional
perspective: Do you have an overgrowth of yeast or other pathogens plaguing your small intestine? How robust is your supply of friendly microbes? Are you producing sufficient stomach acid and pancreatic enzymes to adequately digest your food? How healthy is your gut lining? Stool tests that look at these indicators can also help determine sensitivities and allergies to common dietary irritants, such as wheat, dairy, and soy. The great value of these tests lies in their ability to help you and your practitioner pinpoint your digestive problems to find more targeted solutions. And since so many health issues begin in the gut, by repairing it, you are contributing manifestly to your overall well-being.
Guidelines for Maintaining Healthy Digestion
Once you’ve got a clearer sense of what may be getting in the way of optimal digestion, absorption, or assimilation, you’re ready to go to work. Remember, keeping your inner ecosystem clean is key to preventing cancer from rearing its head.
Keep Things Moving
As with any complex system, your body needs to get rid of its waste on a regular basis, from one to three times a day. Less-frequent evacuation “backs up the tank,” leaving excess toxins behind. Remember, when it comes to helping keep cancer at bay, staying free of toxins is key.
So what does a “perfect” stool look like? Think “The Story of the Three Bears,” featuring Goldilocks: not too soft, not too hard; not too pale, not too dark. Eating a varied Eating for Health diet, with plenty of fiber, should keep things running smoothly. If your bowels still move more slowly than you’d like, try adding an additional 500 to 1,000 milligrams of magnesium, a natural laxative, to your daily regimen.
Get to Know the Bugs in Your Belly
As adults, we all have three to four pounds of bacteria and yeast living within our intestines. This translates to hundreds of trillions of intestinal bacteria, a number that many experts consider to be almost ten times the number of cells in the entire human body (see, for example, Lipski 2005). In a healthy person, more than four hundred species of beneficial organisms flourish in the intestinal tract, aiding in digestion and in the production of B vitamins, vitamin K, and numerous enzymes (Guarner and Malagelada 2003). When health-eroding, pathogenic bacteria get the upper hand, however, we experience digestive distress, impaired detoxification, and increased risk for all diseases, including breast cancer. Your goal is to make sure the beneficial bacteria in your gut far outnumber the pathogenic freeloaders.
MASTERFUL MICROBES: YOUR VERY BEST FRIENDS
The term
probiotic
, a compound of Latin and Greek words meaning “favorable to life,” is popularly used to refer to the helpful bacteria that populate your gut (while technically the term refers to a supplement of these beneficial bacteria). Our ancestors appear to have been well aware of the connection between beneficial bacteria and good health, as we consider the number of age-old fermented foods, rich in healthful bacteria, such as yogurt, sauerkraut, and kimchi, that nourished generations worldwide for centuries.
But every time you take an antibiotic or drink large amounts of chlorinated tap water, you kill off billions of these naturally occurring beneficial bacteria, upsetting the intricate balance of your intestinal terrain. Opportunistic organisms, such as yeast and hostile bacteria, can then flourish, creating a state of imbalance known as
dysbiosis
. The most common type of opportunistic yeast,
Candida albicans
, is a glutton for sugar, which often results in cravings for carbohydrates, such as sugar, pasta, and bread. Prescription antibiotics also modify the natural environment of your intestines; what’s more, the abundance of antibiotics in the meats and other commercial animal products we consume
also
contribute to this intestinal imbalance. This makes the choice of organic, grass-fed, antibiotic-free animal products all the more vital.
GUT FLORA AND ESTROGEN
Recent research has shed intriguing light on the cancer-protective connection between maintaining healthy estrogen levels and healthy gut flora (Boccardo et al. 2006), especially when you consume generous amounts of lignans.
Lignans
are a group of phytonutrients found in seeds, legumes, grains, and vegetables. Flaxseed is by far the richest source of plant lignans, found in the fibrous hull of the seed. Researchers first noted the beneficial activity of flax lignans in the 1980s, when they reported lower levels of lignans in breast-cancer patients than in cancer-free women (Adlercreutz et al. 1986). While the puzzle pieces have not been entirely put together, we do know that when we eat plant lignans, intestinal bacteria convert them into
enterolactones
and
enterodiol
, compounds believed to lower estrogen levels and exert anticancer effects.
AN OUNCE OF PROBIOTICS: A POUND OF CURE?
Making sure you have plenty of healthy bacteria in your gut is a wise investment. If you enjoy fresh yogurt or other fermented foods, you’re already ahead of the game. If not, check out Sally Fallon’s
Nourishing Traditions: The Cookbook That Challenges Politically Correct Nutrition and the Diet Dictocrats
, or Sandor Katz’s
Wild Fermentation: The Flavor, Nutrition, and Craft of Live-Culture Foods
, two excellent books with step-by-step instructions for transforming your diet into a probiotic powerhouse. An alternative is to take a probiotic supplement daily. Look for one with several different strains of bacteria, such as
L. acidophilus
,
L. bulgaricus
,
L. brevis
, and
B. bifidum.
(For a complete list, see
Digestive Wellness
, by Elizabeth Lipski [2005].) If you must take an antibiotic, a course of
saccharomyces boulardii
, a special probiotic yeast supplement sometimes known as “yeast against yeast,” taken along with the antibiotic therapy will help restore equilibrium in your gut, protecting it from the
unhealthy
form of yeast (
Candida albicans
) that commonly plagues people who take antibiotics.
Plugging the Leaks in Leaky Gut
The intestinal tract is lined with cells designed to allow well-digested food to pass through it and to serve as a barrier to pathogens, other undesirable substances, and particles too large to benefit our well-being. Stress, pharmaceuticals, and toxins can slowly wear down this protective barrier, creating a condition called
leaky gut
. Leaky gut leaves a gateway through which undesirable substances can enter the body. This, in turn, can stimulate the immune system to respond in the form of allergies, inflammation, and autoimmune conditions. The longer the leaky gut persists, the longer our intestines “lay out the welcome mat” to both external and internal contaminants. A stool analysis will provide an indication of the state of your gut lining, but your holistic practitioner may also recommend an assessment known as an
intestinal permeability test
. Once it is determined that leaky gut is an issue, there are several steps you can take. The ones that we have found to be successful in our practices include:
- Consuming a varied diet of Eating for Health foods to avoid toxicity and to help keep your intestines at an ideal pH for optimal digestive health.
- Emphasizing fermented foods, which provide healthy bacteria, and fresh fruits and vegetables, which provide just the right
prebiotic
nourishment for healthy bacteria (prebiotics are food ingredients, often fiber, that feed intestinal bacteria). - Avoiding alcoholic beverages, which can interfere with efficient detoxification and put additional strain on the digestive tract.
- Using antibiotics only when absolutely necessary, and carefully heeding the precautions detailed previously.
- Using nonsteroidal anti-inflammatory medications (NSAIDs) sparingly, if at all, because they can erode your delicate gut lining.
- Using a water filter to eliminate chlorine and chloramines from treated tap water.
- Looking out for symptoms associated with common food allergens, such as headaches, bloating, skin eruptions, and brain fog. Ask your practitioner about food-allergy testing if you suspect a problem.
- Taking herbs such as chamomile, yarrow, kudzu, slippery elm, and marshmallow root, and the amino acid L-glutamine to normalize and heal gut mucosa.
- Scheduling relaxation into your life in the same way that you schedule exercise. Putting time aside daily will yield huge rewards.
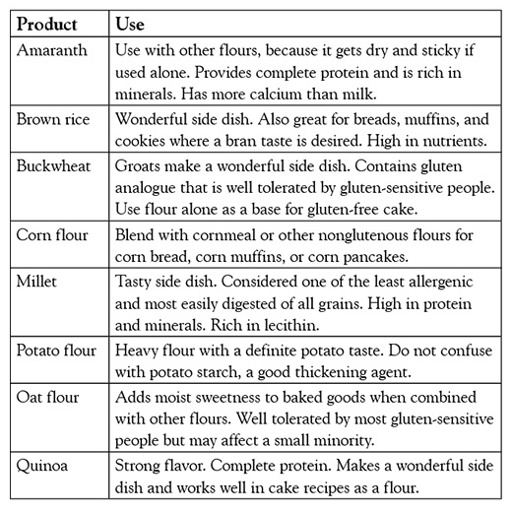
When the Staff of Life Becomes the Stuff of Strife
Gluten intolerance is on the rise. Celiac disease, the most serious form of gluten intolerance, is thought to affect approximately 1 percent of the population, a staggering number in absolute terms and far larger than thought just a decade ago (Fasano et al. 2003). The number of people with some level of sensitivity to gluten in the United States may easily run into the tens of millions. Undiagnosed gluten intolerance or even a mild sensitivity strains your entire system by instigating intestinal and then systemic inflammation. For this reason we encourage you to be aware of whether you are gluten sensitive, and we counsel everyone to keep their gluten intake low. Wheat is by far the most glutenous grain, but barley and rye also contain plenty of gluten. A thorough discussion of the potential problems with gluten is beyond the scope of this book, but in the following table we provide some helpful alternatives to glutenous grains and some tips on how to use them in cooking and baking.
Maximizing Your Digestive Power
By age forty-five or fifty, many of us have stopped producing hydrochloric acid (HCl), the stomach acid we need to thoroughly digest our food. Pancreatic function may have slowed down as well, resulting in less-than-optimal levels of digestive enzymes. These deficiencies often manifest as bloating and other bothersome symptoms, although many people exhibit symptoms that are more subtle and not as clearly related (such as iron-deficiency anemia or weak fingernails). Whether these deficiencies are recognized symptomatically or systematically via medical tests, we suggest taking immediate steps to correct them. For a deficiency of hydrochloric acid (HCl), we recommend the following:
- Take bitter herbs, such as Swedish bitters or a gentian tincture, twenty minutes prior to eating.
- With each meal, drink one teaspoon of apple cider vinegar mixed with warm water, as suggested by Dr. D. C. Jarvis (1958) in his classic book
Folk Medicine: A Vermont Doctor’s Guide to Good Health
, to improve digestion and help with a variety of conditions, including balancing pH. Dr. Jarvis suggests using one teaspoon of honey with each teaspoon of cider vinegar if the vinegar alone is too sour. In most cases, people can tolerate up to 3 teaspoons of each. If you experience any burning sensations anywhere along the digestive tract, it’s best to stop taking vinegar or to neutralize the discomfort by taking baking soda in water or drinking a small glass of milk. - Take an HCl supplement, available at your health food store or through your health practitioner. The amount of HCl a person needs can vary from 30 to 100 grains. Start with one capsule per meal and build to tolerance. A burning sensation in the stomach will tell you that you have taken too much.
Once your HCl is back in check, your pancreatic enzymes should follow suit, since HCl signals the release of these enzymes. However, if you are still symptomatic or continue to test low in HCl, add a pancreatic enzyme supplement at the beginning of each meal. We strongly suggest working with a nutrition consultant or other qualified practitioner to assess your status and to determine the best remedies.
