Women's Bodies, Women's Wisdom (115 page)
Read Women's Bodies, Women's Wisdom Online
Authors: Christiane Northrup
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #Personal Health, #Professional & Technical, #Medical eBooks, #Specialties, #Obstetrics & Gynecology

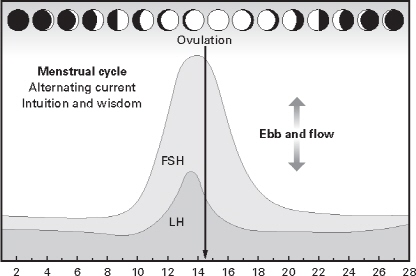
Menstrual cycle (days)
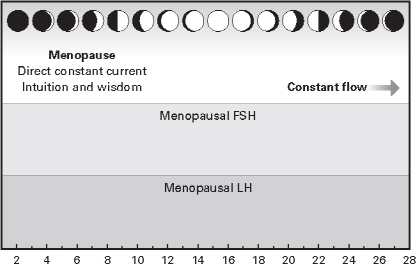
Month (days)
FSH and LH stimulate ovulation and are realized cyclically each month up until the years surrounding menopause. They then undergo a change during which ovulations gradually cease and FSH and LH levels gradually increase.
For years the ob-gyn profession has been steeped in lectures and teaching on “managing” menopause and perimenopause. If a woman’s health care team approaches this life stage with support and respect for a natural process, she will be helped a great deal. But if perimenopause (or any other natural process) is approached from the disease model, with the mind-set that it requires management (and its subtext, control), then a woman’s ability to flourish during and after menopause will likely be undermined. In our culture, the only ages when female endocrine processes escape potential “management” are the years before menarche and after the age of seventy.
Fear of Aging: Symptom of an Ageist Culture
We live in an ageist culture, in which most people believe that it’s natural for aging people to become depressed, fatigued, incontinent, asexual, forgetful, and senile. Pharmaceutical companies and gynecol ogists plant in women seeds of fear that as soon as they go through menopause, their bodies will simply fall apart and waste away unless they are on medication.
An example of this was the cover of a magazine called
Menopause Medicine
from the 1990s. A woman stands by an open window with filmy curtains blowing at her side; only her back is visible. She is looking out on the landscape covered by dead trees and parched earth. The caption under this illustration read, “The Fate of the Untreated Menopause.”
It doesn’t take a degree in psychology to understand how the pharmaceutical companies influence the sensibilities of the average woman or doctor. For most of my career, we ob-gyns felt enormous pressure to give conventional hormone replacement to everyone, having been led to believe that it was necessary to prevent everything from heart disease to osteoporosis. It’s easy to see how the pharmaceutical companies and the media manipulate the stereotypes associated with aging and the deep cultural fears that we women have about them. For decades we’ve been taught that without hormone replacement, we’d lose our attrac tiveness to men; we’d dry up and become brittle, like dry, cracked earth, devoid of moisture and nourishment. Newer research is showing that this doesn’t have to be true.
The experience of aging as we know it is largely determined by beliefs that need updating. Though many people
do
decline with age in this culture, this decline is not a natural consequence of aging—it is a consequence of our collective beliefs about aging. My mother, who is now eighty-five and has never been on estrogen, hiked the entire Appalachian Trail in her late sixties, skied around the base of Mount McKinley shortly thereafter, and spent the summer of 1997 going on a three-month extended hiking and kayaking trip to Alaska. She later climbed the 111 highest peaks in the Northeast with her friend Anne, who is now eighty-seven and chops all of her own wood for heating her house. Another of my mother’s good friends turned ninety in 2005. She and my mother climbed Mount Washington together earlier that year and also went snowshoeing in northern Vermont. Yet as soon as my mother turned sixty, her mailbox was suddenly full of ads for hearing aids, incontinence diapers, and various aids for failing vision, none of which she had any need for. Over time, my mother figured out how to ignore the constant barrage of negative messages about aging. She also told me that though she doesn’t feel much different from when she was thirty, she is definitely treated differently.
Harvard professor Ellen Langer, Ph.D., has extensively researched how the context in which we live influences us to feel either younger or older and can have dramatic consequences for our health. For example, she has found that negative stereotypes about aging set the stage for diminished capacity in older adults both directly and indirectly, while the absence of these same cues prime improved health. Langer and her team looked at women who bear children later in life, curious about whether the youth cues they are given because they are in an environment with mainly younger women would translate into longer lives. That is exactly what they found. Older mothers do, in fact, have longer life expectancies.
4
The good news is that beliefs about age have shifted dramatically in the last decade. As women of the baby boom generation have entered menopause in droves, we are finally seeing many more media images of strong, sexy, vital menopausal women. In fact, today’s menopausal women look younger than ever before. Fifty no longer looks old. In fact, it looks downright sexy on an increasing number of women. The same is true of sixty, as we all saw when Helen Mirren went up to claim her Oscar for the movie
The
Queen
. We are collectively reversing our cultural neg ativity about menopause and aging, one woman at a time. And this change in our beliefs and expectations is showing up in our bodies. For instance, my mother had a health reading from Caroline Myss when she was sixty-eight. Her body read energetically as though she were in her thirties.
The more women ignore ageist stereotypes, the better the chances are that all of us will stay healthy. That’s because we are all connected energetically. And when one woman breaks out of a box of limitation, she makes it easier for the rest of us to do the same. Life expectancy is rising steadily as we collectively change our beliefs about what is possible. People live more than 50 percent longer than they did a century ago, and those working in the life extension field believe that there is no absolute limit to the human life span. Our task at midlife is to realize that our most joyful and pleasurable years can be ahead of us.
CREATING HEALTH DURING MENOPAUSE
To make the most of the menopausal transition, I encourage a woman to think of it as a period during which she’ll be creating the healthy body she needs to last her until the end of life. The menopausal transition is an excellent time to focus on the prevention of problems that, while not necessarily directly associated with menopause, statistically appear to intensify at this stage. At midlife, for example, most women notice that it’s no longer possible to just cut back on bread and desserts for a week in order to take off a few pounds and fit into that little black dress. Nor can we stay up all night without feeling the effects the next day. In short, we can no longer continue to ignore our physical, emotional, and spiritual needs and expect our bodies to stay vital and healthy. It’s time to make proactive lifestyle improvements.
What a woman experiences during this period of her life depends upon a multitude of factors, from her heredity, her expectations, and her cultural background to her self-esteem and her diet. At this time in history, the majority of women in our culture experience some discomfort and some troublesome symptoms at menopause. However, a wide variety of options exists for the treatment of these symptoms, ranging from bioidentical hormones that match those produced in the human female body to homeopathy. The ideal path through the change is one that uses the best of Western medical knowledge concerning hormone metabolism, bone density, and heart health, combined with the comple mentary modalities of the East, from meditation to acupuncture to herbs, to provide optimal individualized care.
Hormone-Producing Body Sites
Though we’ve been taught to think of menopausal symptoms mostly as an estrogen deficiency state resulting from ovarian failure, this belief is based on incomplete information. It is actually progesterone, another hormone made by the ovaries, that is most likely to be deficient during perimenopause, not estrogen. Total well-being at menopause and beyond depends at least as much on having adequate levels of progesterone—as well as DHEA and testosterone, two androgen hormones also produced in the ovaries—as it does on estrogen. Androgenic hormones are associated with sexual response and libido, as well as general well-being, and they are produced not just by the ovaries but by other organs and body sites, too. These include the adrenal glands, the skin, the muscles, the brain, and the pineal gland, as well as hair fol licles and body fat. (see
figure 19
). Interestingly, as hor mone production from the ovaries declines at menopause, a twofold increase in production of androgenic hormones from these other sources takes place. In fact, your body has the ability to make hormones throughout your life. Since androgens can act as weak estrogens and can also be precursors for the production of estrogens, it is clear that the healthy menopausal woman is naturally equipped to deal with hormonal changes in her ovaries. Women who are able to produce adequate levels of androgens in their bodies often sail through menopause quite easily.
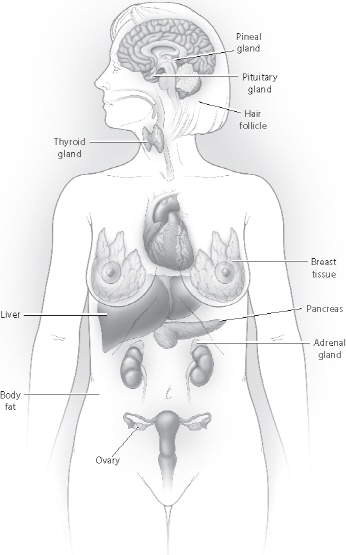
FIGURE 19: HORMONE-PRODUCING BODY SITES
Ovarian estrogen and progesterone levels decrease after menopause. Other body sites, however, are capable of making these same hormones, depending upon a woman’s lifestyle and diet. The female body, therefore, has the capacity to make healthy adjustments in hormonal balance after menopause.
Nevertheless, some women clearly suffer during menopause. While 15 percent of women are symptom-free, a full 85 percent will experience hot flashes, and approximately one-half of this group does not consider the hot flashes to be tolerable. As time goes on, symptoms of vaginal atrophy (thinning of the vaginal tissue) in postmenopausal women tend to increase; heart disease risk and osteoporosis fracture risk also increase but will not be evident until a woman is in her late sixties or older.
Such menopausal problems are due in part to chronic depletion of women’s metabolic resources during the perimenopausal years. The ease of transition into this stage depends upon the strength of a woman’s adrenals and the state of her general nutrition. In a healthy woman, the adrenal glands will be able to gradually take over hormonal production from the ovaries.
Many women, however, approach menopause in a state of emotional and nutritional depletion that has affected optimal adrenal function. And many have had their ovaries removed. Under these conditions, a woman may require hormonal, nutritional, emotional, and/or other support until her endocrine balance is restored.
5
ADRENAL FUNCTION:
WHAT EVERY WOMAN SHOULD KNOW
Our adrenal glands provide us with crucial hormonal support that we all need to go through the day with energy, enthusiasm, and effi ciency. If your adrenals are depleted from chronic overproduction of the stress hormones norepinephrine (adrenaline) and cortisol, you are much more likely to suffer from fatigue and menopausal symptoms. Here are the signs that your adrenals may need attention: You awaken feeling groggy and have difficulty dragging yourself out of bed. You can’t get going without that first cup or two of caffeinated coffee. You rely on sugary snacks and caffeine to get through the day, particularly in the late morning or afternoon. At night, though exhausted, you have difficulty falling asleep as the worries of the day keep replaying in your mind. You wonder what happened to your interest in sex. If this de scribes you, your adrenals may be running on almost empty, even if all your conventional medical tests are normal.
