Breast Imaging: A Core Review (35 page)
Read Breast Imaging: A Core Review Online
Authors: Biren A. Shah,Sabala Mandava
Tags: #Medical, #Radiology; Radiotherapy & Nuclear Medicine, #Radiology & Nuclear Medicine

References: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:122.
Kopans D.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:553–554.
112
Answer D.
Majority of male breast cancer is invasive ductal carcinoma. It usually presents as a firm, tender, subareolar mass typically eccentric to the nipple. Mean diameter at diagnosis is 2.0 to 3.5 cm. Calcifications are uncommon. Diffuse gynecomastia may obscure the cancer. Differential diagnosis includes gynecomastia and fat necrosis.
References: Applebaum A, et al. Mammographic appearances of male breast disease.
Radiographics
1999;19:559–568.
Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging
: Breast. Salt Lake City, UT: Amirsys; 2006;IV:5–54.
113
Answer A.
Apocrine cyst cluster is a cluster of tiny anechoic foci, 1 to 7mm individually with thin intervening septae. No solid components are present. They have a typical appearance on ultrasound. No further intervention/ workup is needed. They are in the lobular portion of the terminal ductal lobular unit (TDLU). One can may see milk of calcium in microcysts. Short-term follow-up can be done if suboptimally seen or individual microcysts are complicated. Biopsy if solid component is present.
Reference: Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging
: Breast. Salt Lake City, UT: Amirsys; 2006;IV:1.
114
Answer 1–B, 2–A, 3–D
.
References: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:183–186.
Nathanson SD, Wachna DL, Gilman D, et al. Pathways of lymphatic drainage from the breast.
Ann Surg Oncol
2001;8:837–843.
115
Answer C.
Phyllodes tumors are uncommon, and most are benign. They usually occur in women in their fifth decade and can be very large when first detected. About 10% of phyllodes tumors are malignant. Most common sites for metastases are the lung and bone. Axillary node metastases are uncommon. Five-year survival is 55% to 75%.
Treatment of choice is wide local exercise for mastectomy for very large tumors. Radiation treatment reduces local recurrence. There is no benefit from chemotherapy.
References: Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging: Breast
. Salt Lake City, UT: Amirsys; 2006;IV:2-96–IV:2–101.
Gordon PB, et al. Solid breast masses diagnosed as FA at fine needle aspiration: Acceptable rates of growth at long term following-up.
Radiology
2003;229(1):233–238.
Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:111–113.
116
Answer A.
The images depict a “shrinking breast,” which is indicative of bilaterality, multicentricity, and multifocality. It represents 10% of all breast cancer. Its size is often underestimated on mammography and ultrasound. Tubular carcinomas have a 95% to 98% 5-year survival rate. Proliferating epithelium in villous-like projections is as seen in papillary carcinomas.
References: Bassett LW, et al.
Diagnosis of Diseases of the Breast
. Philadelphia, PA: WB Saunders; 2005: Chapter 27, 506–507.
Evans WP III, et al. Invasive lobular carcinoma of the breast: Mammographic characteristics and computer aided detection.
Radiology
2002;225:182–189.
Mercado CL, et al. Papillary lesions of the breast at percutaneous core needle biopsy.
Radiology
2006;238:801–808.
117
Answer D.
The mass seen on the MRI is an intramammary lymph node. It is bright on T2-weighted images and demonstrates washout enhancement. It may be possible to see the fatty hilum on nonfat sat T1-weighted images to confirm the diagnosis. Sometimes a vessel can be seen going to the fatty hilum. Correlation with mammograms is also helpful in confirming the diagnosis.
Reference: Morris EA, Liberman L.
Breast MRI: Diagnosis and Intervention
. New York, NY: Springer; 2005:427–431.
118
Answer A.
“Calcific particles” in axillary lymph nodes can be caused by a metastatic calcifying cancer and granulomatous infectious like tuberculosis (TB). Other entities like migrated silicone from implant rupture and gold particles from rheumatoid arthritis therapy may mimic calcifications in lymph nodes. Usually the clinical history can help with the diagnosis. Microcalcifications in lymph nodes rather than pleomorphic calcifications can suggest tuberculous mastitis, but biopsy is needed to exclude metastatic breast cancer.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:304.
119
Answer C.
In cases where there is an explanation for the bilateral axillary adenopathy, such as lymphoma or rheumatoid arthritis, no further evaluation is warranted. If there is no such history, then further evaluation with ultrasound is recommended. In this case, the screening mammogram would be given a BIRADS 0.
Reference: Chelten A, Nicholson B, et al. Is screening detected bilateral axillary adenopathy on mammography clinically significant?
The Breast Journal
2012;18:582–587.
120
Answer D.
When nipple retraction is new, causes may be due to periductal mastitis, duct ectasia, or a malignancy. Cancers that typically occur in the retroareolar region are invasive ductal carcinoma or invasive lobular carcinoma. Both of these cancers, if close to the nipple, can cause the nipple to retract. The first step in the workup of nipple retraction is diagnostic mammography, including spot compression–magnification views in the subareolar region.
References: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:26–36.
Nicholson BT, Harvey JA, Cohen MA. Nipple-areolar complex: Normal anatomy and benign and malignant processes.
Radiographics
. 2009;29(2):509–523.
121
Answer D.
Milk of calcium calcifications are dense and curvilinear on the mediolateral projection. On the craniocaudal projection, they have a smudgy appearance. DCIS calcifications are linear, sometimes branching, and pleomorphic. Skin calcifications often have a calcific rim surrounding a radiolucent center. Oil cysts also have lucent centers.
References: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:73.
Lanyi M.
Diagnosis and Differential Diagnosis of Breast Calcifications
. New York, NY: Springer-Verlag; 1988.
122
Answer A.
The above finding is caused by seat-belt injury. This can be seen in any type of injuries to the breast whether caused by blunt or penetrating trauma. Without a history of trauma, developing densities will be suspicious and may require biopsy. An asymmetry is seen on the left side when trauma is sustained by the driver and on the right by the passenger.
Reference: Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging: Breast
. Salt Lake City, UT: Amirsys; 2006;IV:5–20–IV:5–21.
123
Answer A.
NAT is systemic chemotherapy with or without hormonal treatment of breast cancer prior to definitive breast surgery. Primary goal of NAT is to facilitate clear margins at surgery by clearing skin/chest wall invasion. Size of the tumor is most accurately determined by MRI. Mammography is not very accurate for determining preoperative size of the tumor and is particularly inaccurate for invasive lobular carcinoma.
References: Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging: Breast
. Salt Lake City, UT: Amirsys; 2006;V:1–28–V:1–31.
Yeh E, et al. Prospective comparison of mammography, sonography and MRI in patients undergoing neoadjuvant chemotherapy for palpable breast cancer.
AJR Am J Roentgenol
2005;184:868–877.
124
Answer A.
Lesions requiring surgical excision or rebiopsy after core biopsy include ductal carcinoma in situ (DCIS), atypical ductal hyperplasia (ADH), papillary lesions with atypia, phyllodes tumor, cancer (even if an entire lesion appears to be removed), insufficient samples, and noncongruent results of pathology. Growing PASH should be excised because of overlap with low-grade angiosarcoma. Steatocystoma multiplex consists of multiple, bilateral oil cysts that are benign and do not require excision. A small percentage of phyllodes tumors may be malignant and can sometimes only be diagnosed by a complete histologic examination.
References: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:183–184.
Shah BA, Fundaro GM, Mandava S. Breast Imaging Review:
A Quick Guide to Essential Diagnoses
. 1st ed. New York, NY: Springer; 2010:109.
125a
Answer C.
The mammogram demonstrates diffuse increased trabecular thickening and skin thickening of the left breast which was due to extrinsic compression on the left subclavian vein obstruction from a mediastinal mass.
125b
Answer D.
The mammogram demonstrates diffuse increased trabecular thickening and skin thickening. Main differential diagnoses for these findings are inflammatory carcinoma and mastitis. Clinical symptoms are the key to diagnosis. Punch biopsy to exclude inflammatory carcinoma. Most common agents for mastitis are
Staphylococcus aureus
and streptococcal bacteria.
Reference: Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging: Breast
. Salt Lake City, UT: Amirsys; 2006;V:6–10–V:6–13.
126a
Answer A.
There is a mass seen in the left breast superiorly on the mediolateral oblique (MLO) view with associated calcifications, which needs additional imaging.
126b
Answer B.
Images depict a partially calcified epidermal inclusion cyst. It is a benign cutaneous or subcutaneous epithelial cyst arising from an obstructed hair follicle. Biopsy/fine needle aspiration should be avoided as the contents can be irritating to surrounding tissues, sometimes even leading to abscess formation. They are more common in other parts of the body such as the face, neck, and trunk.
References: Berg WA, Birdwell R, Gombos EC, et al.
Diagnostic Imaging: Breast
. Salt Lake City, UT: Amirsys; 2006;IV:3–16–IV:3–19.
Celik V, et al. Epidermal inclusion cyst of the breast: Clinical, radiologic and pathologic correlation.
Breast J
2004;10(1):57.
127
Answer C.
Thickening of the skin can have many causes. It can be focal or diffuse, unilateral or bilateral. It can occur as a result of tumor invasion, tumor in the dermal lymphatics, or lymphatic congestion by obstruction of lymphatic drainage. Differential diagnosis includes malignancy, infection, nonspecific inflammation, primary skin processes like psoriasis, systemic diseases like scleroderma, dermatomyositis, and causes of vascular obstruction like CHF, superior vena cava syndrome, and anasarca.
Reference: Kopans D.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:339–341.
| 4 | Breast Intervention |
QUESTIONS
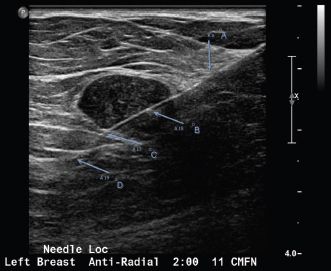
1
A 50-year-old female with a mass is scheduled for ultrasound-guided wire localization. Based on the image below, which letter denotes the wire tip?
Other books
Autopsy of an Eldritch City: Ten Tales of Strange and Unproductive Thinking by James Champagne
Blue Skies by Robyn Carr
Going All In by Alannah Lynne, Cassie McCown
Pound for Pound by F. X. Toole
The Sphere Chronicles: A Holding Kate Series Book by Cole, LaDonna
Fallen Fourth Down (Fallen Crest #4) by Tijan
The Billionaire's Lover: Curves To Keep (Part One) (A BBW Erotic Romance) by Bethany Rousseau
Decision and Destiny by DeVa Gantt
The Troubles of Johnny Cannon by Isaiah Campbell
