Breast Imaging: A Core Review (36 page)
Read Breast Imaging: A Core Review Online
Authors: Biren A. Shah,Sabala Mandava
Tags: #Medical, #Radiology; Radiotherapy & Nuclear Medicine, #Radiology & Nuclear Medicine

A. A
B. B
C. C
D. D
2
You are attempting a stereotactic biopsy on a patient with calcifications very close to the chest wall and difficult to image with the patient prone. What is the best option?
A. Recommend an MRI.
B. Use towels to compress the breast side to side to push the front of the breast out.
C. Retarget to get as close as possible.
D. Place the patient’s arm and shoulder through the hole in the stereotactic table.
3
You are performing an ultrasound-guided biopsy on a patient with a lesion close to the chest wall. Which of the following is the best option?
A. Roll the patient and approach at an angle so the needle is parallel to the chest wall.
B. Explain to the patient the likely risk of pneumothorax.
C. Schedule the patient for wire localization instead.
D. Aim for the periphery of the lesion.
4
Cytologic analysis should be performed for fluid removed during an ultrasound-guided cyst aspiration, if the fluid appears
A. Bright red
B. Green
C. Thick and maroon or dark brown
D. Yellow
5
What is the standard degree difference between the two stereotactic pair images obtained during stereotactic needle biopsy?
A. 20 degrees
B. 30 degrees
C. 50 degrees
D. 60 degrees
6
What is the purpose of using a spinal needle for anesthesia during a stereotatic vacuum-assisted biopsy?
A. To create a tract for the biopsy needle
B. To form the skin wheal
C. To inject beyond the area being biopsied because of the dead space of the needle distal to the sample notch
D. To reduce the burn associated with lidocaine injection
7
You recommend a breast biopsy on a patient but discover she is on aspirin. What is the next best step in management?
A. Counsel patient for increased risk of hematoma/hemorrhage.
B. Cancel biopsy and instead recommend follow-up in 6 months.
C. Stop ASA for 7 days and then biopsy.
D. Do nothing.
8
You perform a stereotactic biopsy, and specimen x-ray demonstrates the calcifications in question; however, pathology reports no calcifications seen. What do you recommend?
A. Recommend repeat biopsy.
B. Follow-up mammogram in 6 months.
C. Recommend surgical excision of the biopsy site.
D. X-ray the pathology blocks and check with polarized light for calcium oxalate.
9
The immediate subareolar area is difficult to adequately anesthetize. Which of the following is the simplest and most effective way to achieve full anesthesia of the nipple areolar complex?
A. Double the amount injected of 1% lidocaine.
B. Apply topical lidocaine to the nipple 30 minutes prior to biopsy.
C. No need to do anything additional.
D. Buffer with sodium bicarbonate.
10
When targeting a lesion for stereotactic core biopsy, images are obtained at +15 and −15 degrees. The images obtained show apparent movement of the target lesion, known as parallax shift. The distance of apparent lesion movement is used to calculate which coordinate?
A.
x
(horizontal)
B.
y
(vertical)
C.
z
(depth)
11
An axial CT image of a postlumpectomy patient is shown. What is the most common complication of breast surgery?

A. Abscess/infection
B. Hemorrhage
C. Lymphedema
D. Necrosis
E. Seroma
12
What is the best technique to attempt if the stereotactic needle is in the breast at the appropriate depth and the lesion is too far from it?
A. Completely withdraw the needle out of the skin and make a second skin opening.
B. Change only the
z
coordinate.
C. Change the
x
and
y
coordinates after retargeting the lesion.
D. Cancel the procedure.
13a
A 42-year-old female presents for a screening mammogram. Thin linearbranching calcifications were noted in the left upper outer breast, new from a prior study. There is no family history of breast cancer. The patient is asymptomatic. What is the appropriate next step?
A. Clinical breast exam to detect any underlying masses
B. Stereotactic biopsy
C. Referral to surgery for excisional biopsy
D. Additional mammographic imaging
E. Short-term 6-month follow-up to assess stability
13b
What is the appropriate BI-RADS category?
A. BI-RADS 0
B. BI-RADS 1
C. BI-RADS 2
D. BI-RADS 3
E. BI-RADS 4
13c
After diagnostic mammogram, calcifications were noted to span a distance of 6 cm. What is the next appropriate step?
A. Refer to surgery for lumpectomy.
B. Refer to surgery for left breast mastectomy.
C. Refer to surgery for left breast mastectomy and preventative right breast mastectomy.
D. Stereotactic biopsy
14
Which one of the following patients can still be qualified for radiation therapy?
A. Patient with multicentric or diffuse disease
B. Pregnant patient
C. Patient who has had previous radiation therapy
D. Patient with collagen vascular disease
E. Patient with axillary lymphadenopathy
15
Which of the following is considered a contraindication to breast-conserving therapy (lumpectomy and radiation)?
A. Breast cancer diagnosed in the third trimester of pregnancy
B. Axillary metastases
C. Prior history of radiation and lumpectomy in the contralateral breast
D. Two or more separate tumors in different quadrants of the same breast
16
Stereotactic biopsy of the following calcifications was performed. Specimen radiograph confirmed that two calcifications were present in the specimens.
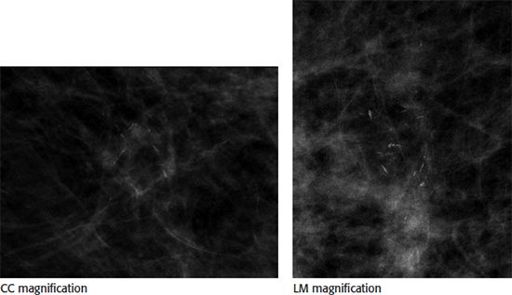
Core biopsy pathology results returned as “benign, fibrocystic changes with microcalcifications.” What is the next most appropriate step?
A. Annual screening mammogram
B. Recommendation for surgical biopsy
C. 6 month follow-up postprocedure mammogram
D. Repeat stereotactic biopsy
E. Breast MRI
17
A patient presents prior to a planned lumpectomy for wire localization of a 3-cm extent of previously biopsied, known malignant, calcifications in the left breast. The best course of action is
A. Place a wire in the center of the calcifications
B. Place a wire at one of the margins of the calcifications and provide measurements and instructions to the surgeon on what nearby tissue to excise
C. Place two wires, using the bracketing technique, at each edge of the calcifications
D. Cancel the procedure and call the surgeon, this extent of disease is too large for lumpectomy and mastectomy should be considered
18
Of the following choices, which needle biopsy device is considered most effective for use during stereotactic-guided breast biopsy of microcalcifications?
A. 14-gauge or smaller gauge spring loaded
B. 14-gauge or smaller gauge vacuum assisted
C. 11-gauge or larger gauge spring loaded
D. 11-gauge or larger gauge vacuum assisted
19
What is the most appropriate indication to perform galactography?
A. Single duct nonspontaneous and spontaneous bloody, milky, or clear nipple discharge
B. Single duct spontaneous bloody, milky, or clear nipple discharge
C. Single duct nonspontaneous and spontaneous bloody, serous, or clear nipple discharge
D. Single duct spontaneous bloody, serous, or clear nipple discharge
E. Single duct spontaneous bloody, serous, or milky nipple discharge
20
A mammographic wire localization is being performed for biopsy-proven invasive ductal carcinoma. The distance from the tip of the needle to the mass is 3 cm. Based on the image below, what is the next most appropriate step?
Other books
Hot for Teacher by Dominique Adair
A Study In Scarlet Women by Sherry Thomas
Marked by Pedro Urvi
Daddy Dearest by Heather Hydrick
The Lighter Side of Life and Death by C. K. Kelly Martin
Gideon's Spear by Darby Karchut
The Wisdom of Perversity by Rafael Yglesias
Antiques Fruitcake by Barbara Allan
Midnight Whispers - Paranormal Romance by Bullard, Catherine
