Digestive Wellness: Strengthen the Immune System and Prevent Disease Through Healthy Digestion, Fourth Edition (43 page)
Authors: Elizabeth Lipski

Lactoferrin in our eyes helps prevent infection by binding to iron, which is needed for the growth and survival of disease-causing microbes. It also appears to inhibit the development of biofilms in the eyes. In addition, lactoferrin may help control oral biofilm development and is useful in people with gingivitis. Conversely, depleted levels of lactoferrin in the sinuses increase biofilm development and recurring sinus infections. You can increase lactoferrin levels by supplementing with whey, colostrum, or transfer factor.
Dental research leads the way in the field of what works with people. Dental research shows promise with use of polyethylene glycol, chlorexidine, and sodium hypochlorite in breaking up the biofilms that develop on our teeth, in root canals, and in other oral tissues. Some integrative physicians are using chelation therapy with ethylenediaminetetraacetic acid (EDTA) to break up biofilms, although it hasn’t been shown to be terribly effective in dental biofilm research.
Integrative physicians have also been experimenting with a three-step approach to eradicating disease-causing biofilms. In stage one they combine the use of enzyme products such as protein-splitting enzymes like serrapeptase, nattokinase, and proteases with oral EDTA and lactoferrin. They follow this with antibiotic treatment with either herbs or medications, and finally use insoluble fibers, charcoal, and pectin to clean up the debris. I have heard good case reports but have not seen any large-scale studies on this approach yet.
Remember that biofilms can be normal and healthy too; eradicate them only under the supervision of a clinician skilled in this area. We don’t yet understand all of the ramifications of treating them.
9
Fire in the Gut: Immune and Inflammation
“Our bodies respond to trauma or infection in a predictable manner, a phenomenon called inflammation. … Whether the stimulus is a laceration, a burn, or an inhaled speck of pollen by a person with atopic syndrome, a remarkably similar combination of signs is elicited.”
—Robert Rountree, M.D.
“The gut immune system has the challenge of responding to the pathogens while remaining unresponsive to food antigens and the commensal flora. In the developed world this ability appears to be breaking down, with chronic inflammatory diseases of the gut commonplace in the apparent absence of overt infections.”
—Thomas T. MacDonald and Giovanni Monteleone,
“Immunity, Inflammation, and Allergy in the Gut”
The function of the immune system is to determine what is you and what is not you: self from nonself. When exposed to a stimulus or event that your immune interprets as nonself, it begins sending warriors to the rescue. Current research indicates that 70 percent of the immune system is located in or around the digestive system. This is because of the enormous amount of food and drink that we ingest, which is “foreign” material that needs to be sorted.
Ninety-nine percent of the time, it is the immune system’s job
not
to respond. We develop what is called tolerance for our environment. Otherwise each time you ate an orange or inhaled some pollen your immune system would be activated, much like the boy who cried wolf. Your body has recognition of what is similar to yourself and what’s not. When you eat foods high in antioxidants, nutrients, and polyphenols (colors), your immune system sighs, “All is well.” But what if we eat foods that
aren’t really foods: soft drinks, trans fats, artificial colors and flavors, and other food chemicals? Immune research indicates that our reaction to these is one of “nonself,” which activates the immune system.
Figure 9.1
illustrates the basic mechanism of an immune response.
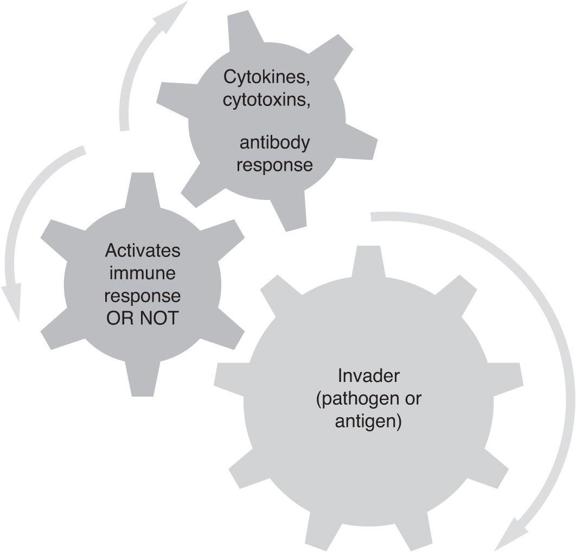
Figure 9.1
Basic immune response.
The external manifestation of an immune system out of balance is inflammation, which we experience as swelling, heat, and/or pain. This reaction could be triggered by hay fever, a sprained ankle, acid reflux, or eating foods that disagree with us. In fact, inflammation is now believed to be the underlying cause of obesity, high blood pressure, diabetes, atherosclerosis, Alzheimer’s disease, Parkinson’s disease, cancer, depression, and more.
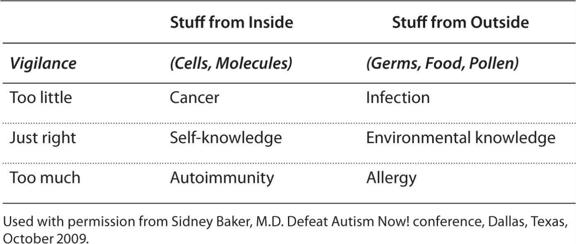
Throughout your body, you have a continual communication that balances inflammation and healing. We are always walking a dance between just the right amount of immune surveillance and inflammation, and not feeling well. When challenged, the immune system mounts a predictable response that is proportional to the threat. (See
Table 9.1
.) It produces inflammatory molecules such as cytokines; interleukins; chemokines; secretory IgA; IgG, IgE, and IgM antibodies; and others.
Table 9.1
Causes and Degrees of Immune Vigilance
When you think about inflammation and immune imbalances in the digestive system, consider pain and discomfort: acid reflux; sores in our mouths; periodontal disease; inflammatory bowel diseases, such as Crohn’s and ulcerative colitis; irritable bowel syndrome; and dysbiosis. Also included are autoimmune diseases, such as type 1 diabetes, celiac disease, multiple sclerosis, lupus, Sjögren’s disease, and rheumatoid arthritis. Inflammatory bowel diseases result from an exaggerated immune response to what would be normal bacteria in someone who has different genes. The main function of probiotics is to modulate the immune system. Beneficial microbes help to keep “bad” microbes in balance. (See
Chapter 27
, “Autoimmune Diseases.”) In the chapter on probiotics, you learned that one of the main benefits of pre- and probiotics is that they modulate the immune system. When we have a balance of probiotic, commensal, and few disease-causing bacteria, there is a balance between inflammation and healing. (See
Figure 9.2
.) When we have a lot of disease-causing microbes and few probiotic bacteria and commensal bacteria to balance that out, it leads to inflammation, pain, and disease.
Your immune system has four basic parts. Your body’s first response typically is to watch and be tolerant. When something unusual occurs, the immune system has an ordered way of responding that layers your defenses from simplest to most dire and then hopefully back to health again.

Figure 9.2
How probiotics and prebiotics modulate the immune system.
(The original is from Mazmanian, S. K., Round, J. L., & Kasper, D. L. [2008]. “A Microbial Symbiosis Factor Prevents Intestinal Inflammatory Disease.”
Nature
, 453[7195], 620–625.)
 Innate immune system:
Innate immune system:
This is your first line of defense against things that your body generally doesn’t like, such as cancer cells, mold, mildew, yeast, and viruses. It responds quickly and within minutes or hours to deal with bacteria, viruses, parasites, and other threats that can make you sick. Typically this is called a T-helper 1 cell response (Th-1 response). Some of the responses that are produced include interferon, defensins, lysozyme, complement (which activates the body to attack and kill cells), mast cells, polymorphonuclear lymphocytes, macrophages, dendritic cells, phagocytes, lactoferrin, reactive oxygen species (like hydrogen peroxide and superoxide radical), natural killer cells, and the interleukins IL-2, IL-12, and IL-18.
 Adaptive immune system:
Adaptive immune system:
The second line of defense is your adaptive immune system. This is a slower response and is specific. Your body makes a more careful examination to determine whether this is a friend or foe and then develops a specific response that is appropriate. This mainly comprises allergic responses. So, perhaps the first time you are stung by a bee, it’s not so bad. But then your body remembers that insult and the next time you have a huge allergic reaction.
If you are allergic to peanuts, your body produces an antigen that is specific to peanuts. Or if you have had the measles, your body will produce antibodies that are specific to measles. This is to help protect you from invaders with a long-term response. This level of immune response is also where food and environmental sensitivities reside. Typically this is a T-helper 2 (Th-2) response, where a specific response occurs to a specific challenge. Other cells involved are the antibodies IgA, IgM (memory antibodies), IgG (delayed sensitivities), IgE (allergy); T- and B-lymphocytes; and the interleukins IL-4, IL-5, IL-10, and IL-13.
 Immune-inflammatory response:
Immune-inflammatory response:
In this response your body overreacts and begins responding to your own tissues as if they were foreign. A combination of your own genetics plus your environmental exposures plus your overall immune balance will determine whether you trigger an autoimmune response. Increased intestinal permeability often plays a role in autoimmune conditions. For example, people with celiac disease typically have HLA-DQ2 or HLA-DQ8 positive genes. When these people are exposed to gluten-containing grains along with a leaky gut, the grain triggers an immune and inflammatory response that is celiac disease. In other diseases, such as rheumatoid arthritis (RA) and ankylosing spondylitis (AS), genes (HLAB-27) meet bacteria (proteus in RA or klebsiella in AS), which sets off the immune response. The antibodies to these bacteria, which are typically non-disease-causing in most of us, set up an autoimmune response that causes inflammation, pain, and tissue destruction in people with the “right” genes and environment. In type 1 diabetes, either a virus or food sensitivities can trigger the disease. These are typically Th-17 responses and produce the interleukins IL-1, IL-17, and IL-22 and tumor necrosis factor alpha (TNF-alpha).
