Examination Medicine: A Guide to Physician Training (82 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

Note:
Subarachnoid haemorrhage occurs in 3% of patients as a result of intracranial aneurysm. As this is an autosomal dominant condition, all family members of patients with polycystic kidney disease should be assessed for kidney disease. Cerebral aneurysms can be screened for in patients with kidney disease by MRI, in the absence of a previous history of subarachnoid haemorrhage.
Table 16.20
Some other causes of abdominal masses
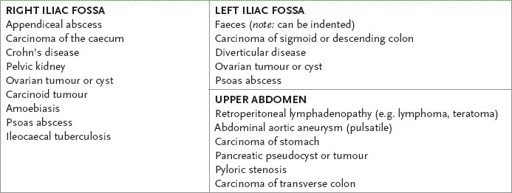
Table 16.21
Causes of splenomegaly
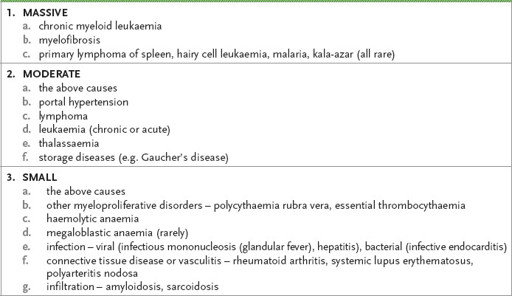
Note:
Secondary carcinomatosis is a rare cause of splenomegaly.
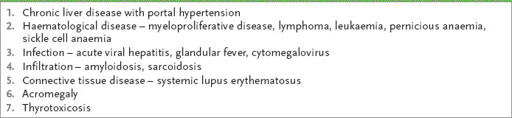
Table 16.22
Causes of hepatosplenomegaly
5.
Carefully feel for the kidneys bimanually. Remember that any left-sided mass may arise from a number of sites.
HINT
Bimanual palpation of the kidneys (balloting) will not work unless the hand under the patient is placed vertically (almost to the spine).
HINT
If you have found hepatosplenomegaly, always consider the possibility of associated polycystic kidneys (a common trap for young players in the test).
6.
The usual distinguishing features of a spleen compared with a kidney are as follows.
a.
The spleen has no palpable upper border.
b.
The spleen has a notch.
c.
The spleen moves inferomedially on respiration.
d.
There is usually no resonance over a splenic mass.
e.
The spleen is not bimanually palpable (i.e. not ballottable).
f.
A friction rub may occasionally be heard over the spleen.
7.
Percuss for ascites as a routine. If the abdomen is resonant out to the flanks on percussion, do not roll the patient over. Otherwise, look for shifting dullness. The technique is usually performed by percussing away from your side of the bed until you reach a dull note, then rolling the patient towards you and waiting at least a short time before percussing again for resonance.
8.
Always auscultate briefly over the liver, spleen and renal areas. Listen for bruits, rubs and a venous hum. Note the presence of bowel sounds. An arterial systolic bruit over the liver is usually caused by either hepatocellular carcinoma or acute alcoholic hepatitis. A friction rub over the liver may be caused by tumour, recent liver biopsy, infarction or gonococcal perihepatitis (rather unusual); splenic rubs indicate infarction. A venous hum occurs uncommonly in portal hypertension.
HINT
If you are asked to examine the gastrointestinal system rather than the abdomen, begin by examining the hands and go on to the arms, face, chest, abdomen and legs as described (see
Table 16.16
).
9.
Examine the groin next. Palpate for inguinal lymphadenopathy. Always ask if you may palpate the testes.
10.
If you now suspect liver disease, you must go on and look for the peripheral stigmata of chronic liver disease. In this instance, it is probably better to proceed from the abdomen to the chest wall. Look for gynaecomastia, spider naevi (
Fig 16.34
), hair loss (in men) and breast atrophy (in women). Examine the breasts if you suspect intra-abdominal malignant disease.
FIGURE 16.34
Chronic liver disease (spider naevi). J J Kanski.
Clinical ophthalmology: a synopsis
, 2nd edn. Fig 24.23. Elsevier, 2009, with permission.
a.
Now sit the patient at 45° and measure the JVP so as not to miss constrictive pericarditis as a cause of cirrhosis. Palpate anteriorly for supraclavicular nodes, then sit the patient forwards and feel posteriorly for the other cervical nodes. Look at the back for sacral oedema and spider naevi. If ascites is present, examine the chest for pleural effusions.
b.
Look at the face next. Note any scleral abnormality (jaundice, anaemia or iritis) and look at the corneas for Kayser-Fleischer rings. Xanthelasma are common in patients with advanced primary biliary cirrhosis. Feel for parotid enlargement, which may be present soon after an acute alcoholic binge. Inspect the mouth with a torch and spatula for angular stomatitis, ulceration and atrophic glossitis. Smell the breath for fetor hepaticus.
c.
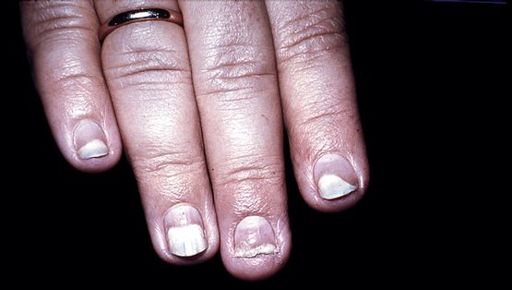
Look at the arms for bruising and spider naevi. Next examine the hands. Ask the patient to extend his arms and hands and look for evidence of hepatic flap. Look also at the nails for clubbing and white nails (leuconychia) (
Fig 16.36
), and note any palmar erythema and Dupuytren’s contractures (the latter are associated with alcohol or trauma) (
Fig 16.35b
). The arthropathy of haemochromatosis may also be present (a degenerative arthritis that particularly involves the second and third metacarpophalangeal joints).
FIGURE 16.35
(a) Dupuytren’s contracture of the foot. (b) Dupuytren’s contracture of the hand.
FIGURE 16.36
Liver nails (leuconychia).
Clinics in Dermatology
, Fig 3. May/June 2008. 26(3):296–305.
d.
Next examine the legs for oedema, bruising and any rashes. If you have found Dupuytren’s contractures in the hands, look for similar tendon thickening and shortening on the soles of the feet (
Fig 16.35
); Dupuytren’s contracture of the foot. Look for the nervous system signs of alcoholism – namely, peripheral neuropathy, proximal myopathy, cerebellar syndrome, Wernicke’s encephalopathy (bilateral VI nerve palsies) and Korsakoff’s psychosis.
HINT
Do not hurt the patients while examining them.
e.
Candidates are almost always stopped well before this stage. Do not forget to ask to perform a rectal examination and urine analysis. Also ask to look at the temperature chart. Ask whether you may further examine for hernias by asking the patient to stand and cough.
11.
If, on the other hand, you have found signs consistent with a haematological problem, proceed as described in that section.
12.
If you find a pulsatile liver, examine the cardiovascular system and particularly note any other signs of tricuspid regurgitation.
13.
If an enlarged kidney is present (see
Table 16.19
), ask to check the blood pressure and the urine.
14.
If malignant disease is suspected, examine all the node groups, the lungs and the breasts after a thorough abdominal examination. Non-haematological malignant disease that causes hepatomegaly rarely leads to splenomegaly unless the portal vein is directly involved.
HINT
Haemochromatosis, an autosomal recessive disorder, is an important cause of liver disease. Consider this diagnosis if any of the following signs are present:
•
pigmentation (bronze)
•
arthropathy (typically degenerative arthritis of the MCP joints of the index and middle fingers, but any other joint may be involved; pseudogout may occur)
•
testicular atrophy (owing to iron deposition in the pituitary gland)
•
dilated cardiomyopathy
•
glycosuria (as a result of diabetes mellitus).
The haematological system
The haemopoietic examination
‘This 75-year-old man has had problems with tiredness. Please examine his haemopoietic system.’
Method (see
Table 16.23
)