Examination Medicine: A Guide to Physician Training (86 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

2.
Have the patient stand or sit on the side of the bed. Look at the hands. Look for coarse features and spade-like shape, as well as increased sweating and warmth. Osteoarthritis-like changes are frequent in the hands, shoulders, hips and knees. Perform Phalen’s wrist flexion test for the carpal tunnel syndrome (median nerve entrapment). Feel the ulnar nerve for thickening at the elbow.
3.
Go to the arms and test for proximal myopathy. Also look in the axillae for skin tags (molluscum fibrosum), greasy skin and acanthosis nigricans (brown-to-black velvety elevation of the epidermis owing to multiple confluent papillomas).
4.
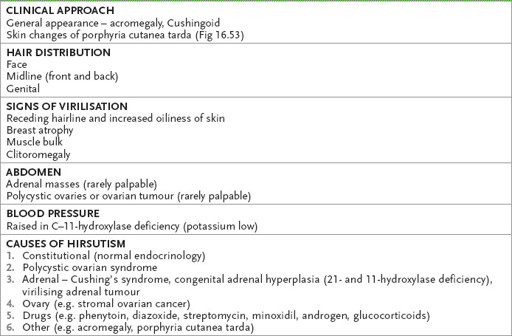
Go on to the face. Look for frontal bossing as a result of a large supraorbital ridge (which may also occur in rickets, Paget’s disease, hydrocephalus or achondroplasia). Note whether there is a large tongue (sometimes too big to fit into the mouth neatly). Enlargement of the lower jaw (called prognathism) and splaying of the teeth may be present. Notice any acne or hirsutism in women (see
Table 16.44
) and test the voice, which may be deep, husky and resonant.
Table 16.44
Hirsutism
5.
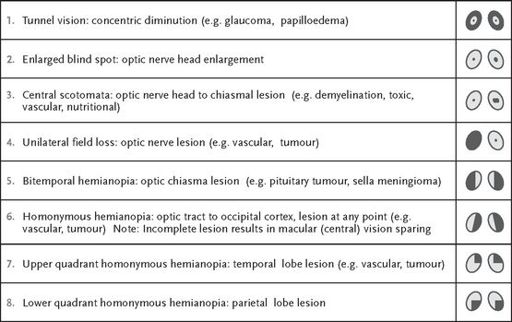
The eyes must be carefully examined. Visual fields should be checked – look particularly for bitemporal hemianopia, but many field defects are possible (see
Fig 16.86
). Examine the fundi for optic atrophy, papilloedema and angioid streaks (red, brown or grey streaks three to five times the diameter of the retinal veins appearing
to emanate from the optic disc and owing to degeneration of Bruch’s membrane with resultant fibrosis). There may also be diabetic or hypertensive changes.
FIGURE 16.86
Visual field defects associated with lesions of the visual system.
Causes of angioid streaks (PASH)
P
aget’s disease, pseudoxanthoma elasticum (
Fig 16.47
), poisoning (lead)
FIGURE 16.47
Pseudoxanthoma elasticum. Plucked chicken skin appearance on neck is characteristic of pseudoxanthoma elasticum. M Yanoff, J S Duker, J J Augsburger et al.
Ophthalmology
, 3rd edn. Fig 6-35-7. Elsevier, 2009, with permission.
A
cromegaly
S
ickle cell anaemia
H
yperphosphataemia (familial)
6.
Examine the thyroid gland for diffuse enlargement or a multinodular goitre.
7.
Examine the cardiovascular system for signs of congestive cardiac failure, the abdomen for organomegaly – of liver, spleen and kidney – and for signs of hypogonadism (secondary to an enlarging pituitary adenoma).
8.
Examine the lower limbs for osteoarthritis and pseudogout. Large osteophyte formation and ligamentous laxity are common features. Also look for foot drop (entrapment of common peroneal nerve) and heel pad thickening.
9.
If there is time, look for evidence of hypothyroidism and adrenocortical insufficiency (from an enlarging pituitary adenoma).
10.
Do not forget to ask for the results of a urine analysis to exclude glycosuria secondary to glucose intolerance and take the blood pressure (hypertension is an association). Decide whether the acromegaly is active (see
Table 16.36
). Ask whether any photographs taken of the patient over the years are available for inspection (typically, manifestations begin in middle age). See
Table 16.37
for the diagnostic evaluation.
Table 16.36
Evidence of activity in acromegaly
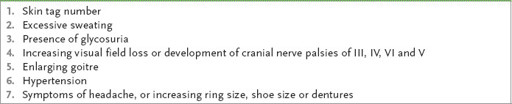
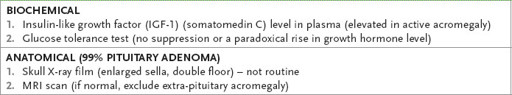
Table 16.37
Diagnosis of acromegaly
Addison’s disease
‘This 65-year-old woman has weakness, anorexia and weight loss. Please assess her.’
Method
Fortunately, you suspect Addison’s disease.
1.
Ensure the patient is appropriately undressed and look for pigmentation (
Fig 16.48
) (particularly in the palmar creases, elbows, gums and buccal mucosa, genital areas and scars) and vitiligo (
Fig 16.49
), owing to an autoimmune disease association. Ear lobe calcification occurs rarely.
FIGURE 16.48
Hyperpigmentation in Addison’s disease compared with a normal patient. W D James.
Andrews’ diseases of the skin: clinical dermatology
, 11th edn. Fig 24.3. Saunders, Elsevier, 2011, with permission.
FIGURE 16.49
Vitiligo. R A Spritz. The genetics of generalised vitiligo and associated autoimmune diseases.
Journal of Dermatological Science
, 2006. 41(1):3–10, Fig 1.
2.
Take the blood pressure and test for a postural drop. Ask for the results of a urine analysis, as diabetes is associated with Addison’s disease. Remember that the rest of the autoimmune cluster may also be associated (see
Table 16.38
) and consider the possible causes (see
Table 16.39
). Diagnostic tests are summarised in
Table 16.40
.
Table 16.38
Autoimmune-associated disease
| Addison’s disease | Primary ovarian failure |
| Hypoparathyroidism | Pernicious anaemia |
| Mucocutaneous candidiasis | Vitiligo |
| Diabetes mellitus (type 1) | Alopecia |
| Hashimoto’s thyroiditis | Hypophysitis |
| Graves’ disease | Myasthenia gravis |
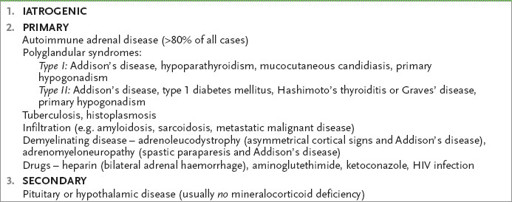
Table 16.39
Causes of Addison’s disease (chronic adrenal insufficiency)
*