Murder and Mayhem (26 page)
Authors: D P Lyle

Of course, the patient/victim could survive this event or not, as you wish. Either way is plausible. If he is to survive, the surgeon must give the warmed blood and fluids rapidly, close up any of the coronary arteries he had been working on, close up the patient's chest, and get him to the ICU as quickly as possible. Meanwhile, the biomedical people would work frantically to repair the machine.
This is good stuff, an exciting scene.
What Dose of Morphine Would Kill a Man Undergoing Cancer Treatment?
Q: My victim is in the final stages of metastatic lung cancer and is taking morphine intravenously at home, administered by a pump. For a 145-pound male who is seventy-six years of age, what might a typical dosage be? Would twice that amount cause a deadly overdose?
A; Metastatic lung cancer can be a very painful disease. Cancers that originate in the lung often metastasize (spread) to the liver, the brain, and the bones. In medical jargon these metastatic lesions are often referred to as "mets." Brain mets tend to enlarge within the closed space inside the skull and also cause swelling of the surrounding brain tissue. The net effect is a rise in intracranial (inside the skull or cranium) pressure. This can cause severe continuous headaches. Mets to bones such as the ribs and the spine can be extremely painful. For this reason narcotics such as morphine sulfate (MS), Demerol, Dilaudid, and others are commonly used. In an individual with terminal cancer the risk of addiction is of little concern.
The chosen analgesic (pain reliever) may be given by intermittent injections or by use of one of the automated methods. Continuous infusion pumps and patient-controlled analgesia (PCA) are commonly employed in this circumstance. The former is by definition a continuous infusion of fluid containing the sedating drug, usually MS. PCA is a system of IV delivery that allows the patient to control the timing of delivery within preprescribed parameters. Here, a syringe filled with the MS is placed in an automatic injector that is attached to the patient's IV line. The injector delivers a prescribed amount of the drug when the patient depresses a handheld button. Parameters are set to limit the amount that can be
requested per hour. Within these limits, the patient may use as much or as little as he feels is necessary.
As with many medications, the dosing of MS is determined by the patient's weight. The dosing schedule in most patients ranges from 0.2 to 0.4 milligram (mg) per kilogram (kg) of body weight per hour and then is titrated (a gradual increase in dose) upward as needed. Since one kilogram equals 2.2 pounds, your 145-pound (66 kg) patient would require approximately 13 to 26 mg per hour. However, in patients who have been on the continuous drip or PCA for weeks or months, tolerance to the drug develops, just as it does in addicts. Therefore, larger and larger doses are needed to obtain the same sedating and pain-relieving effect. Some patients in this situation require doses as high as 500 mg per hour, which is enough to kill even the strongest person not habituated to the drug.
In large doses MS depresses respiration and drops the blood pressure. If enough is given, the recipient will stop breathing, his blood pressure will fall to dangerously low levels, and he will die from apnea (absence of breathing) and shock. The dose required to kill someone depends on the rate of delivery, the underlying medical condition of the victim, and whether the victim has developed tolerance to the drug.
Doubling the dose at any given level may or may not be enough to be lethal. For example, if a patient was receiving 60 mg per hour and the rate was doubled to 120 mg per hour, it probably wouldn't do him in, though it certainly could do in a debilitated man with terminal lung cancer. Raising it to 240 mg per hour (quadruple) probably would work. A half hour to two or three hours at this increased rate may be required to do the victim in.
On the other hand, if given as a single injection, an extra 20 to 40 mg might be enough. Since the person on a drip of 60 mg per hour receives 1 mg per minute, giving 20 to 40 mg over a few seconds is a large increase in dose and would probably work. MS works rapidly, within a minute or so, when given as a bolus (a single, rapid injection), so you are actually increasing the dose from 1 mg per minute to 41 mg per minute—a huge increase that would likely cause apnea and shock almost instantaneously.
So either markedly increasing the rate of administration (by increasing the drip rate or the concentration of the drug per cubic centimeter of fluid, or both) or giving a bolus of the drug would accomplish your goal in this situation.
Additionally, patients with lung cancer often have sicker lungs, not just from the cancer itself but from surgery that removes part or all of one lung and radiation therapy or chemotherapy, which may damage the good lung tissue. In this case, even smaller amounts might work.
I suggest either quadrupling the rate or giving 40 mg as an IV bolus, depending on which scenario fits your story best.
Can a Transfusion Reaction Be Used for Murder?
Q: In my story an elderly and seriously ill man is murdered by a nurse who switches the blood he is to receive, causing a reaction that kills him. How does this reaction occur, and what symptoms would the victim have?
A: Transfusion reactions come in many varieties. They may be as mild as a rash or perhaps chills and fevers, or be so severe as to cause death. First let's look at why these reactions occur.
The red blood cells (RBCs) are the carriers of oxygen from the lungs to the tissues and of carbon dioxide from the tissues to the lungs. This is accomplished by using the hemoglobin inside the RBCs. The RBCs also have antigens on their surface, and they are at the root of transfusion reactions.
These antigens are designated either A or B. From these our blood-typing system (ABO system) has been derived. Type A blood lias only A antigens, type B only B antigens, type AB both, and type O neither.
Simple, so far. But the serum of the blood (the liquid part) also carries antibodies. It is the reaction of these antibodies with the antigens of the transfused blood that causes problems.
Type A serum (that is, the serum of people with type A blood) has anti-B antibodies. Type B has anti-A antibodies. Type AB has neither. Type O has both anti-A and anti-B antibodies.
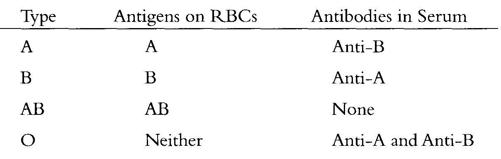
Reactions occur when blood with the right antigen is given to a person with the its corresponding antibody. For example, if a type A person (who has anti-B antibodies in the serum) receives type B blood (which has the B antigen on its RBCs) or type AB blood (which has both A and B antigens), an adverse reaction will occur because the anti-B antibodies in the recipient's serum will react with the B antigens on the transfused RBCs. This is a transfusion reaction. The result is agglutination, or clumping, of the blood cells and the release of several harmful chemicals that cause the symptoms and signs of this basically "allergic" reaction.
It gets more complicated than this because there are other antigen/ antibody problems with blood matching such as the well-known Rh factor, which is either positive or negative, and many others, mostly named after the physicians that discovered them. Your blood type is typically expressed only in terms of the ABO and Rh systems. For example, a person who is A-positive has type A blood and the Rh factor antigen is present, while a person who is O-negative has type O blood and the Rh factor is absent.
Because of the multitude of potentially problematic antigens, blood is typed and cross-matched prior to transfusion. This tests the blood that is to be given directly against the recipient's blood to determine if any antigens and antibodies exist that might cause the blood to be incompatible and thus lead to reactions. In very emergent situations such as gunshots, stabbings, or automobile accidents where the victim is bleeding to death and there isn't time to do a complete cross-match, type-specific blood is given. A person's blood type can be determined in a few minutes, but cross-matching may take hours. In these cases a type A person receives type A blood, and everyone hopes for the best.
In your story I would suggest that you have your victim be type A and have the nurse switch the blood to type B. This would definitely cause a reaction. The patient would develop fever, chills, and a diffuse, irregular red rash over his entire body. This could begin within minutes or be delayed for a few hours. This type of reaction would not likely result in death.
However, your victim could develop a full-blown anaphylactic allergic reaction, which would be the above symptoms plus swelling of the face, lips, hands, and feet, shortness of breath, low blood pressure, and severe shock with pallor, cold and clammy skin, and a bluish tinge (called cyanosis) to his lips, fingers, and toes. He would ultimately suffer cardiac arrest and death. Since this represents the severest form of allergic reaction, anaphylaxis would develop fairly quickly after the blood was infused.
If the victim survived an anaphylactic reaction, there is a strong probability that his kidneys would be severely and irreparably damaged, requiring dialysis. This damage results from the kidneys' attempt to filter the clumped RBCs from the blood. The iron found in the hemoglobin molecules of the RBCs is particularly toxic to the kidney tissues.
Can a Bee Sting Kit Be Altered to Result in the Death of the User?
Q: I have a scene in which someone who is allergic to bee stings dies after being given a shot from his bee sting kit. Is there a substance that when combined with medicine in the bee sting remedy would prove fatal?
A: The deadly allergic reaction that follows bee stings in susceptible individuals is called anaphylaxis. It is a severe allergic reaction that causes spasm of the lung's bronchial tubes (breathing airways), which basically causes a severe asthmatic attack with shortness of breath and wheezing. Anaphylaxis also is associated with a profound drop in blood pressure, leading to shock. Without treatment, death can quickly follow.
Common causative agents of anaphylaxis and other allergic reactions include antibiotics (penicillin, sulfa), local anesthetics (lido-caine, procaine), antisera (gamma globulin, tetanus), foods (nuts, shellfish, eggs), iodine (used in certain X-ray exams), and insect stings (yellow jacket wasps, honeybees, fire ants). When an allergic individual is exposed to the allergenic substance, the reaction may be immediate and profound.
The emergent treatment is an injection of epinephrine (adrenaline), which is the substance in the bee sting kits that allergic persons should keep on hand. Epinephrine reverses many of the allergic processes immediately. The person is then transported to the hospital, where further treatment is carried out that typically consists of oxygen, medications for blood pressure support, antihistamines (such as Benadryl), and steroids.
One way to do the victim in would be to replace the epinephrine with water. He would then succumb to the bee sting.
Another way would be to tamper with the concentration of the epinephrine. Reducing it would probably not work since the net effect would be a partial treatment, which might be enough to allow the victim to reach the hospital. It would be better to increase the concentration.
Epinephrine is basically speed. If given in large amounts, it can cause marked elevation of the blood pressure and deadly changes in cardiac rhythm that can kill almost instantly. The emergency bee sting kits are called Epipen Auto-Injectors and contain 0.3 cc of epinephrine at a 1:1000 dilution. This means that each cc of the medication contains 1 milligram (mg) of epinephrine. Thus, the delivery of 0.3 cc yields a dose of 0.3 mg.
Increasing the dose by a factor of five or ten—a dose of 1.5 to 3 mg—could cause the desired result (cardiac arrhythmia and death), especially if given intravenously. In your scenario, giving either multiple injections (not practical) or tampering with the drug concentration in one of the injectors would do this. Substituting a more concentrated solution of epinephrine could work. The beauty of this approach is that no new drug is required, and the coroner might assume that the victim died from the standard dose of epinephrine, which can rarely happen, or from the allergic reaction itself. Of course, if the coroner tested the residue in the auto-injector, he would likely be able to determine that the concentration of the drug had been altered. But maybe not.
If you want to add another drug, any speedlike product would do the trick, since the effect of the epinephrine and the other drug would be additive. Many of these are readily available. Cocaine (basically a speedball when mixed with an amphetamine such as epinephrine), crystal methamphetamine, and perhaps the rave drug Ecstasy, which is methylenedioxymethamphetamine, would work.
