Oxford Handbook of Midwifery (144 page)
Read Oxford Handbook of Midwifery Online
Authors: Janet Medforth,Sue Battersby,Maggie Evans,Beverley Marsh,Angela Walker

- Gently press her thumb and fingers together, release the fingers and repeat in a rhythmic pattern (Fig. 24.4)
- Sometimes it is helpful to press inwards and back towards the chest wall while squeezing
- The fingers should be repositioned at intervals to allow drainage from all the lactiferous ducts.
The length of time for expressing depends on the reason why the mother is expressing. If she wants to express all the milk she can from the breast, she should continue until the flow subsides.

The mother may express from the second breast by repeating the above process. A mother who wishes to express as much milk as possible should continue to switch between breasts for as long as milk is being obtained.
1,2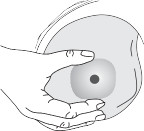
Fig. 24.3
Make a c-shape with finger and thumb.682
CHAPTER 24
Breastfeeding
Fig. 24.4
Expressing breast milk.Breast pumps
Mothers who use a mechanical pump may find they are able to express larger volumes, especially if using an electrical pump.
1Numerous pumps are available to hire or buy, but they fall into three types:
- A hand pump
that is mainly for relieving the breasts. These are usually of simple design and work on a simple vacuum principle. They are not suitable for expressing milk which is to be stored and given to a baby because they can not be sterilized effectively.
1 •
•
Battery-operated pumps
vary widely in design, all produce a rhythmicvacuum, although some are also designed to give a degree of compression. Some mothers find these pumps useful if they are expressing on a regular basis, as they are less tiring than a hand pump.
- Electric pumps
are usually heavy and bulky and therefore less portable. As they are efficient, they are commonly used within hospitals, but they are usually shared by several mothers and therefore maintenance and cleanliness are essential. Ideally all mothers should be given their own equipment for the machine, which should include a collection beaker, tubing, and sterilizing equipment.
1Using breast pumps
Women may find that their let-down reflex is more difficult to induce with a pump than with hand expressing. Massaging the breast and hand expressing for a short time prior to using the pump may help. A photo- graph, item of the baby’s clothing or toy may also help.
EXPRESSION OF BREAST MILK
683
Dual pumping
Dual pumping is when both breasts are expressed at the same time. This can be done either by hand expression or using a pump. It has been shown to shorten the time required for expressing and increases the mother’s prolactin levels.
1
If using a pump, a Y coupling is required. It is particularly helpful if a large amount of milk is required, e.g. with twins and multiple births, or if there is a need to increase the milk supply rapidly.Principles of expression
Establishment of lactation:
- A hand pump
- Expression should commence as soon as possible after the birth.
- Express frequently, 6–8 times in 24h, more if possible.
- Express at least once during the night.
- Avoid set patterns of expressing, instead aim to imitate the irregular feeding pattern adopted by most babies.
If lactation is already established, and there is a need to express to maintain lactation because of separation of the mother and baby, the last three of the above principles should be applied. It is important to remember that expressing does not provide the same stimulus to the breast as the baby suckling, and the milk supply may begin to diminish. If this is the case, the mother should be encouraged to increase the number of expressions.
To increase the milk supply, for example if the baby is not feeding sufficiently or if the mother wishes to build up a milk supply before returning to work, the mother should be encouraged to:
- Express after and/or between feeds or, if the baby is not feeding, to increase the number of expressions
- Express at least once in the night
- Avoid set patterns of expressing; rather, expressing whenever she can. It takes appropriately 24h for the supply to increase.
Recommendations for storage of breast milk
For use in the home
3
- Fresh breast milk can be:
- Kept for up to 5h at room temperature
- Stored in a refrigerator at a temperature 2–4°C for up to 5 days.
- Kept for up to 5h at room temperature
- If milk is not to be used within 24h, freezing is recommended:
- Milk can be kept frozen in an ice-making compartment for 2 weeks
- Milk can be kept safely up to 6 months in a domestic freezer.
- Milk can be kept frozen in an ice-making compartment for 2 weeks
- Any plastic container that can be sterilized and made airtight, is suitable for storing breast milk. Many commercial products are available.
3Storing breast milk for use in hospital
- Some types of plastic are not suitable for storing breast milk for preterm or sick babies.
- Use up-to-date guidelines, e.g. UK Association for Milk Banking Guidelines,
4
for advising mothers which containers to use and how to store the milk. - Hospitals often pasteurize milk for use in a milk bank but this is not usually necessary if the milk is for the mother’s own baby.
CHAPTER 24
Breastfeeding684
Reheating expressed breast milk at home
- Frozen milk can be:
- Thawed slowly in a refrigerator but must be used within 24h or discarded
- Thawed at room temperature and used immediately
- Thawed slowly in a refrigerator but must be used within 24h or discarded
- Frozen milk should never be thawed or heated in a microwave.
5 - Some prefer to warm the milk to body temperature.
- Never re-freeze breast milk.

- UNICEF UK (2004).
Breastfeeding Management Course
. London: UNICEF UK Baby Friendly Initiative. - Breastfeeding Network (2004).
Expressing and Storing Breast Milk Leaflet
. Paisley: Breastfeeding Network. - UNICEF/Department of Health (2007).
Off to the Best Start
. London: DH. Available at: M www.
dh.gov.uk/publications (accessed 12.4.10). - United Kingdom Association for Milk Banking (2001).
Guidelines for the Collection, Storage and Handling of Breastmilk for a Mother’s Own Baby in Hospital.
London: United Kingdom Association for Milk Banking (UKAMB), Queen Charlotte’s and Chelsea Hospital. - Sigman, M. Burke KI, Swarner OW, Shavlik GW (1989). Effects of microwaving human milk.
Journal of the American Dietetic Association
89
(5), 690–2.This page intentionally left blank
CHAPTER 24
Breastfeeding686
Breastfeeding and returning to work
Mothers who are returning to work may find this a stressful time, espe- cially if they are breastfeeding. The longer a mother breastfeeds, the more benefits there are for both mother and baby. Mothers may wish to con- sider different working options, e.g. part-time work, job sharing, working different hours, working partly at home. Health professionals should give mothers information and assistance to try to make the return to work as easy as possible.
Three practical ways to combine breastfeeding and work are:
- UNICEF UK (2004).
- Expression of breast milk while at work
- Childcare near the mother’s place of work
- Partial breastfeeding.
There are advantages and disadvantage to all three options and it will depend upon the mother’s circumstances which option is most appro- priate for her.
If the mother decides to express breast milk at work, she will need to:
- Practise expressing milk prior to returning to work (if possible she should wait until breastfeeding is fully established, when the baby is about 2 months old). The expressed breast milk (EBM) can be stored in the freezer to give the mother a back-up supply
- Ensure she has equipment for expressing at work, which will include a pump, storage containers, sterilizing equipment, spare breast-pads, and a cool bag for transportation (many commercial products are being produced now to make this easier for mothers)
- Consider dual pumping, as this reduces the time required to express
- Have spare batteries and vacuum seals at work if using a pump
- Ask at work for the following facilities:
- Use of a room that is warm, clean, and has a lockable door
- Facilities for hand washing
- Somewhere clean to leave equipment for sterilizing
 • Use of a fridge to store EBM
• Use of a fridge to store EBM - A low comfortable chair
- Use of a room that is warm, clean, and has a lockable door
- Store milk safely.
The law relating to breastfeeding at work
In the UK, mothers do not have statutory rights to paid breastfeeding breaks, but do have certain legal protection under the health and safety laws. While breastfeeding, she and her baby have special health and safety protection, the same as that for a pregnant woman. However, to use this protection she must inform her employers in writing. Employers are also obliged to provide ‘suitable facilities’ where breastfeeding employees can ‘rest’. If the woman is working with hazardous substances, the employer should take appropriate actions to make the job safe. If this is not possible, an alternative job should be offered or she should be suspended on full pay.
1When to express
This will depend upon the individual and the type of work, but also depends upon the employer’s attitude. It is not essential to have regular breaks, as it is better to aim to imitate the irregular feeding pattern that most babies adopt.
BREASTFEEDING AND RETURNING TO WORK
687
Childcare near the mother’s workplace
If the baby is in childcare near the mother’s place of work, the mother could visit the baby during breaks and breastfeed normally. Although this is the best option, it may prove difficult to demand feed around working hours, and the baby may be upset by the mother coming and going.
Partial breastfeeding
This is when the mother breastfeeds normally when at home but the baby receives formula milk while the mother is at work. This can work very well when the mother is unable to express or visit the baby. However, her milk supply may diminish and she may still have to continue with formula feeds for those feeds that are normally missed when working. Partial breastfeeding is not possible before the milk supply is fully established at around 2 months.

1
Maternity Action (2009).
Information Sheet: continuing to breastfeed when you return to work
. London: Maternity Action. Available at: M
www.maternityaction.org.uk/workingparents.html (accessed 12.4.10).CHAPTER 24
Breastfeeding688
Discontinuation of breastfeeding
The DH recommends exclusive breastfeeding for the first 6 months (26 weeks) of an infant’s life, and 6 months is the recommended age for the introduction of solid foods for infants.
1
However, the time when mothers discontinue breastfeeding is very variable and depends upon many factors. Sudden cessation should be avoided if possible to maximize the mother’s comfort and to avoid mastitis. The mother should be advised to slowly drop one feed at a time, allow several days before dropping a further feed, and to feed on alternate days when down to one feed. This helps the milk supply to adjust and allows the milk to diminish naturally. There are circumstances that need special consideration.Mother going into hospital
- If possible, arrange for the baby to accompany the mother and continue feeding.
- A family carer may need to assist the mother with baby care if the hospital can not provide assistance.
- If this is known in advance, the mother can express and freeze EBM, especially if she is to undergo a general anaesthetic.
- The mother needs to ask about equipment and facilities for expressing, sterilizing, and storing breast milk. She may need to take in her own pump.
- If a mother has to stop feeding temporarily due to medication, the supply can be maintained by expressing.
- The mother should ask if safe alternative drugs are available.
Baby going into hospital
- If possible, the mother should accompany the baby.
- If not possible, e.g. because of other children at home, the mother should express and send the milk to the hospital.
- If the baby is unable to suckle and/or receive breast milk, the mother
 should express to maintain the supply and reduce the risk of mastitis.
should express to maintain the supply and reduce the risk of mastitis. - If stopping breastfeeding, this should be done gradually.
Sudden cessation, due to cot death or illness
- A small amount should be expressed, just to relieve pressure.
- Support the breasts well with a firm bra, binding has not been shown to help and may increase the risk of mastitis.
- Use cold compresses.
- Mild analgesics, e.g. paracetamol, may help relieve the discomfort.
- Slightly reduce fluids, but do not drastically reduce fluids as this may temporarily increase the supply.
1
Department of Health (2004).
Infant Feeding Recommendations.
London: HMSO.This page intentionally left blank
CHAPTER 24
Breastfeeding690
Breastfeeding problems
A problem-solving approach should be taken when managing common breastfeeding problems. This should include;
- Listening to the mother
- Taking a breastfeeding history. Use of the UNICEF BFI Breastfeeding Assessment Form is advised
1 - Observing a breastfeed
- Offering information on appropriate solutions and alternatives to enable a mother to make her own decision
- Offering the ongoing support of a breastfeeding peer supporter.
Sleepy/non-feeding baby
There are a number of reasons why a baby will not feed in the first few days following delivery and these include:
- Drugs given to the mother in labour, e.g. pethidine and epidural
- Unpleasant experience at the breast, e.g. force applied to the head when fixing
- Frustration as a result of not obtaining nourishment due to poor fixing at the breast
- Jaundice
- If possible, arrange for the baby to accompany the mother and continue feeding.
- Frozen milk can be:
Other books
The Scarlett Legacy (Woodland Creek) by Lee, K.N., Woodland Creek
Ritos de muerte by Alica Giménez Bartlett
Cuts Like a Knife: A Novel (A Kristen Conner Mystery Book 1) by M.K. Gilroy
Be My Victim and other Strange Tales from the Cape by Andre Beerwinkel
The Columbus Affair: A Novel by Steve Berry
Seize the Night: New Tales of Vampiric Terror by Kelley Armstrong, John Ajvide Lindqvist, Laird Barron, Gary A. Braunbeck, Dana Cameron, Dan Chaon, Lynda Barry, Charlaine Harris, Brian Keene, Sherrilyn Kenyon, Michael Koryta, John Langan, Tim Lebbon, Seanan McGuire, Joe McKinney, Leigh Perry, Robert Shearman, Scott Smith, Lucy A. Snyder, David Wellington, Rio Youers
The Disorderly Knights by Dorothy Dunnett
Porn - Philosophy for Everyone: How to Think With Kink by Dave Monroe, Fritz Allhoff, Gram Ponante
Midian Unmade by Joseph Nassise
