Pediatric Primary Care Case Studies (75 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

• All children from low socioeconomic status families
In most of these situations there are cofactors of rapid growth and deficient nutritional states. These commonly occur together, making the child more susceptible to the depletion of iron at a time when the body has greater need for it. Some information regarding ethnic backgrounds can help point toward specific explanations for aberrant blood findings. Oswaldo’s history reveals many of these risk factors.
Pathophysiology of Anemia
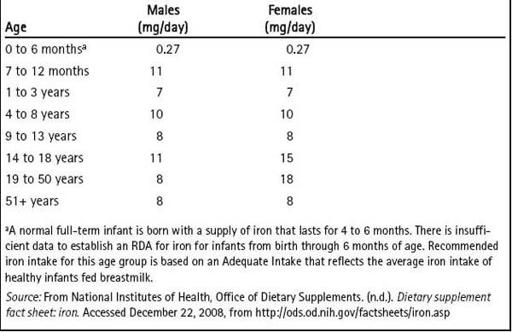
Anemia is defined as a low hemoglobin level in the blood. The physiologic impact of anemia on a growing child can be devastating. The human brain undergoes rapid and fundamental development during the first 2 years of life; therefore, lack of nutrition, as seen with decreased oxygen transportation in iron deficiency anemia (IDA), results in life-long cognitive sequelae when occurring during this critical period. Iron deficiency occurs gradually. Dietary requirements for iron are noted in
Table 19-4
.
In the
prelatent phase
the body’s iron stores are depleted. During the
latent phase
, the serum iron and iron-binding capacity decrease below normal levels. Latency is also associated with reduced erythropoiesis that is reflected in a decreased mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH) and an increase in the red cell distribution width (RDW) as iron deficiency alters red cell size unevenly. It is during the
frank phase
that anemia is evident through direct hematologic studies, noted through decreases in hemoglobin (Hgb) and hematocrit (Hct) (Berman, 2004; Lesperance, Wu, & Bernstein,
2002). Early identification of anemias and intervention are essential for mitigating irreparable effects.
Table 19–4 Recommended Dietary Allowances for Iron
a
Anemia results from an imbalance between the destruction and production of red blood cells. In IDA, the iron stores are depleted to the extent that the hemoglobin essential to red cell production is no longer adequate for this to happen. Decreased red blood cell (RBC) production typically occurs gradually and causes chronic anemia. Any of several mechanisms may be responsible for this decreased production: bone marrow failure, impaired erythropoietin production, and defects in the maturation of red cells. Hemolysis, or increased RBC destruction, may be triggered by extracellular causes: mechanical injury (such as in hemolytic–uremic syndromes or cardiac valvular defects), antibodies (as from autoimmune disorders), infections, drugs, toxins, and thermal injury to RBCs (as in severe burns). Hereditary causes tend to decrease RBC production due to intracellular defects, including defects in cell membrane, enzyme defects, hemoglobinopathies, thalassemias, porphyrias, and paroxysmal nocturnal hemoglobinuria. Blood loss, either acute or chronic, represents the last category of decreased RBC production and can result from disease processes or trauma (Lesperance et al., 2002; Lee & Truman, 2007).
There are three kinetic categories of red blood cells used to describe anemias:
microcytic
, indicating undersized red blood cells;
normocytic
, indicating normal sized red blood cells; and
macrocytic
, referencing cells that are larger than normal. The second characteristic used to differentiate the types of anemia refers to the amount of hemoglobin contained in cells. When the hemoglobin is low, the anemia is referred to as
hypochromic
.
Oswaldo’s history of acquired pallor, bluish sclera, lack of activity, and a diet of mostly cow’s milk with no other significant iron source makes iron deficiency the most likely etiology of his anemia. His health history reveals many risk factors for iron deficiency anemia as well: low socioeconomic status, immigrant, age, diet, and appearance. This diagnosis is further suggested by the physical presence of glossitis and stomatitis.
Conditions with Anemia as a Symptom
IDA is classified as a
microcytic
and
hypochromic
anemia and is the most common of the anemias. Iron deficiency is the most common nutritional deficiency, and IDA is its most severe expression (Centers for Disease Control and Prevention [CDC], 2002). Children between 6 and 20 months, preterm infants, and menstruating adolescent females are at the greatest risk in general, but the incidence doubles in Mexican Americans and African Americans (Borgna-Pignatti & Marsella, 2008).
Thalassemia is another microcytic, hypochromic anemia, though it is most often encountered in its minor or trait variation. The thalassemias are genetically transmitted, with homozygous disease having the greatest health impact. Thalassemia minor is important to differentiate from iron deficiency anemia because thalassemia does not respond to iron therapy. It occurs with greater prevalence among certain racial and ethnic groups. Alpha-thalassemias are
most prevalent in persons of Southeast Asian descent, whereas the beta-thalassemias are found among persons of Southeast Asian, Middle Eastern, or Mediterranean descent. Symptoms may appear between 3 and 6 months of age. Information gathered from the family medical history, such as anemia, miscarriage, jaundice, gallstones, or splenomegaly, should further raise the index of suspicion. Laboratory studies help to differentiate thalassemia minor from anemia. The Mentzer index is determined by dividing the MCV by the RBC count. A score greater than 13 suggests iron deficiency anemia, whereas less than 13 is indicative of thalassemia. The free erythrocyte protoporphyrin (FEP) test is another lab that is useful in differentiating the two anemias: a microcytic anemia with an elevated FEP rules out a diagnosis of thalassemia; however; it does not confirm the diagnosis of iron deficiency anemia. For a definitive diagnosis, hemoglobin electrophoresis is necessary, with a quantitative A2 and F hemoglobin. Beta-thalassemia trait will show elevations of either or both A2 and F hemoglobin (Garfunkel, Kaczorowski, & Christy, 2007).
Celiac disease is another common cause of iron deficiency (10–30% of cases) because it decreases the body’s ability to absorb up to 46% of ingested iron. The only other disorder to equal this significant level of malabsorption is small bowel resection. Disorders that lead to decreased acid secretion, such as
H. pylori
, also impede iron absorption. Situations leading to blood loss (polyps, ulcers, hemorrhagic telangiectasia, and diverticulitis) also deplete iron stores, as do parasitic infestations (Irwin & Kirchner, 2001). After all other causes for a microcytic anemia have been ruled out, there is the possible explanation of anemia of chronic disease, which is only a diagnosis of exclusion.
It is interesting to note that in children with breath-holding spells there is a high incidence of iron deficiency anemia and that the rate of occurrence of these spells decreases following a therapeutic trial of elemental iron supplementation (Borgna-Pignatti & Marsella, 2008). Anemia in combination with leukopenia, neutropenia, or thrombocytopenia is more suggestive of failure of RBC production caused by conditions such as aplastic anemia, Fanconi anemia, or leukemia (Lee & Truman, 2007). This information underscores the need to seek the cause of anemia in order to provide the definitive treatment. Anemia is a symptom of an underlying disorder. As the anemia diagnosis narrows, the diagnosis of the underlying disorder then needs further treatment.
What physical findings in Oswaldo are suggestive of iron deficiency anemia?
Relying solely on physical examination to make a diagnosis of iron deficiency anemia is not very reliable because the findings are nonspecific and often late manifestations, including pallor, fatigue, glossitis, edema (due to milk-induced protein-losing enteropathy with iron deficiency), spoon nails, angular stomatitis, bluish tint to sclera, irritability, frontal bossing, exercise intolerance, abnormal immune response, growth retardation, impaired collagen synthesis (blue sclera), epithelial abnormalities (gastrointestinal mucosal lesions, spoon-shaped nails), and chewing ice. Tachycardia is noted as a poor
compensation for an acute process, such as blood loss. A normal heart rate is suggestive of a chronic process. Jaundice may be seen in the face of a hemolytic process as bilirubin accumulates. Splenomegaly occurs as a result of malignancies, acute infections, inherited hemolytic anemia, or the case of hypersplenism secondary to portal hypertension (Hermiston & Mentzer, 2002; Lesperance, Wu, & Bernstein, 2002).
What aspects of the history indicate risk factors for lead toxicity?
The following are aspects of Oswaldo’s history that are risk factors for lead toxicity:
• Pica (eating non-nutritive substances)
• Crawling (increases amount of time on floor where residue accumulates)
• Mouthing behavior (young children explore their worlds)
• Age (toddlers are at increased risk due to floor play and hand–mouth exploration)
• Lower socioeconomic status
• Residing in an old building (lead paint was used until 1978 and still is utilized in some nonresidences and military installations [CDC, 2002])
• Wearing a medal on a chain—composition unknown
What physical findings would one look for in cases of suspected lead toxicity?
Lead Poisoning
Children with lead poisoning can be without symptoms until levels rise high enough to result in permanent neurologic damage. Lethargy may be noted in children with mild levels and perhaps a complaint of abdominal pain. As the severity of poisoning increases, diffuse abdominal, even colicky pain becomes evident. For serum lead levels > 300 mcg/dL, expected signs may include lethargy, nausea, vomiting, green or tarry stools, hypotension, rapid pulse, metabolic acidosis, shock, coma, hepatic necrosis, renal failure, and local gastrointestinal erosions. The nonspecific nature of these symptoms underscores the need for a high level of suspicion and an organized environmental history. Encephalopathies occur more commonly in children than in adults. These encephalopathies are characterized by seizures, mania, delirium, and even coma. A horizontal line across the nails or gumline may be evident, though such lines are in evidence so rarely as to have little clinical significance (Roberts & Reigart, 2002). As with other anemias, there may also be pallor. On radiograph, lead fragments may be visible in the gut, and uptake lines may appear on long bones, but these measures are indicated in a more severe presentation of toxicity.

