Pediatric Primary Care Case Studies (94 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

Making the Diagnosis
What is the most likely diagnosis regarding Emma’s syncopal episode?
You have arrived at your diagnosis of neurocardiogenic syncope/vasovagal-related syncope using an algorithmic approach to the emergent evaluation of syncope in children and adolescents, as outlined in
Figure 23-1
. This algorithm provides a systematic method to assess the etiology of a syncope episode in a child or adolescent and serves as a practice guide that the healthcare provider can quickly use in either the ED or primary care setting.
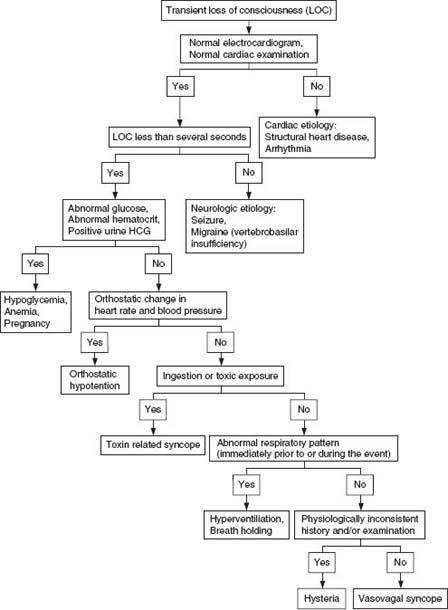
Figure 23-1 Emergent evaluation of syncope in children and adolescents.
Source:©
2008 UpToDate.
Management
Does Emma need further specialty referrals or admission to the hospital?
Indications for Referral or Admission
The majority of children, like Emma, who have had syncope with a negative evaluation can be followed as outpatients. Concerning features such as absence of a significant prodrome, palpitations or chest pain, a family history of syncope or sudden death, and recurrent episodes should be referred for further cardiac evaluation. Follow-up consultation with a neurologist should be considered for children with prolonged loss of consciousness and/or a history of focal neurologic findings.
Admission to the hospital for further evaluation and observation should be considered under the following circumstances:
• Evidence of cardiovascular disease
• An abnormal ECG
• Chest pain
• Cyanosis
• Apnea or bradycardic spells that resolve only with vigorous stimulation
• Abnormal neurologic findings
• Orthostatic hypotension that does not resolve with fluid therapy
Emma’s clinical presentation and subsequent findings meet none of the criteria for admission to the hospital for additional observation or testing.
Best Practice Evidence for Managing Emma’s Syncopal Event
Now that you have thoroughly evaluated Emma’s syncopal event using data obtained from her history, physical examination, and first line diagnostic studies using a systematic approach to data collection, and having come to your diagnosis of neurocardiogenic syncope (vasovagal), you are ready to discuss this event and its likely etiology with Emma and her mother.
Emma’s mother is very upset after all the questions and many tests, which seem to her to indicate that Emma might have a “heart condition.” What will you tell her?
It is important that Mrs. Kaplan, Emma, and her coach understand that Emma does not have a heart problem. There are no family risk factors such as a family history of early cardiac death (less than 45 years of age), sudden deaths including unexplained accidents involving a single motor vehicle or drowning, known arrhythmia (long QT syndrome), and familial cardiomyopathy. In addition, syncope that occurs during physical exertion is very concerning for a cardiac etiology, whereas syncope after exertion may occur with vasovagal syncope or cardiac conditions (Driscoll et al., 1997). Emma passed out
after
physical activity, which is more consistent with a noncardiac etiology. A normal ECG is one of the most important tests to evaluate syncope. Emma’s ECG is normal, indicating the unlikelihood that Emma has a heart condition.
It is documented that up to 15% of children experience a syncopal episode prior to the end of adolescence (Lewis & Dhala, 1999), and that fainting is a transient loss of consciousness, which typically occurs after activity. Similarly, Emma’s symptoms match patients who have had vasovagal syncope. Prior to the event and her loss of consciousness, Emma changed position, going from the huddle to standing. She reported feeling dizziness, lightheadedness, sweating, nausea, and weakness, and had blurred vision. Her loss of consciousness was short with no postictal state/prolonged unconsciousness, and she did not have seizure activity or loss of bladder or bowel control. These are Emma’s exact symptoms and are due to vasovagal syncope.
Emma wants to know if she can return to sports tomorrow. What will you tell her?
Emma may return to sports tomorrow. She should take the following precautions:
Increase fluids intake and avoid dehydration.
Increase salt in diet.
Assume sitting/supine position at onset of symptoms.
Avoid noxious stimuli (i.e., avoid hot environment or prolonged standing/kneeling).
Address anxiety/stress/emotional concerns.

