Pediatric Primary Care Case Studies (96 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

Viral and bacterial pneumonia occur throughout the year; however, they are more prevalent in fall and winter. Many speculate that during cooler months there is enhanced person-to-person droplet spread of respiratory pathogens due to crowding, along with diminished host resistance due to impaired mucociliary clearance from dry indoor air (Durbin & Stille, 2008).
Children who have underlying cardiopulmonary disorders and other medical conditions are at higher risk for pneumonia and its complications.
These conditions include congenital heart disease, bronchopulmonary dysplasia, asthma, sickle cell disease, gastroesophageal reflux, and acquired immunodeficiency disorders. Also, children exposed to cigarette smoke are at higher risk for acquiring pneumonia as a result of impaired mucociliary clearance and increased risk of aspiration. In addition, the use of alcohol has been associated with increased colonization of the oropharynx with aerobic gram-negative bacilli (Durbin & Stille, 2008).
Table 24–1 Childhood Community-Acquired Pneumonia: Common Pathogens | |
| Age | Pathogen |
| 3 weeks to 3 months | Chlamydia trachomatis |
| | Respiratory syncytial virus |
| | Parainfluenza |
| | Streptococcus pneumoniae |
| | Bordetella pertussis |
| 3 months to 4 years | Respiratory syncytial virus |
| | Parainfluenza |
| | Human metapneumovirus |
| | Influenza |
| | Rhinovirus |
| | S. pneumoniae |
| | Mycoplasma pneumoniae |
| 5 years through adolescence | Mycoplasma pneumoniae |
| | Chlamydophila pneumoniae |
| | S. pneumoniae |
| | Mycobacterium tuberculosis |
Clinical Manifestations
Typical clinical findings of pneumonia depend somewhat on the infecting agents. Bacterial and viral pneumonias occur at all ages and can have an acute or gradual onset with mild URI symptoms a few days beforehand. In contrast, mycoplasmal pneumonia typically occurs after 5 years of age and tends to have a slow onset. A temperature of ≥ 102°F (≥ 39°C), chills, cough and dyspnea are suggestive of bacterial pneumonia. Viral pneumonias commonly have a slower onset and a less prominent fever compared to what occurs with bacterial pneumonia. Cough, wheezing, and stridor may also be found in viral pneumonia. A dry persistent cough, a prodrome of chills, headache, sore throat, gastrointestinal complaints, and malaise are characteristic of mycoplasmal pneumonia (Brady, 2009).
What diagnoses would you consider with this history and physical examination?
Differential Diagnosis
You consider the following diagnoses:
• Bronchiolitis
• Foreign body aspiration
• Cystic fibrosis
• Asthma
• Tuberculosis
These are the typical conditions to consider. Other possibilities, although remote in this case, include congestive heart failure, acute bronchiectasis, and pulmonary abscess.
Given those diagnostic possibilities, what other information would help you make the diagnosis?
From the above review, some other information you should obtain includes the following:
• History of previous episodes of respiratory illness (immuncompromised)
• History of travel
• History of contacts with confirmed or suspected infectious tuberculosis
• History of choking (foreign body aspiration)
• History of foul smelling stools (cystic fibrosis)
• Results of prior purified protein derivative (PPD) skin testing (tuberculosis)
• History of animal exposure/insect bites
Mr. Dixon reports that Mary has no previous history of pneumonia or significant respiratory illness—just the usual colds. The family has no history of recent travel nor a history of contacts with confirmed or suspected TB infections. Her PPD skin test was negative at 12 months of age. Mary has not experienced any episodes of choking, and her stools are not foul smelling. The family does not have pets, and she has not had contact with animals and has had no recent insect bites.
Physical Examination
Vital signs: Temperature 103°F, pulse 130, respiratory rate 32, O
2
saturation 96% on room air. Her weight is 23 kg (75th percentile) and length is 115 cm (95th percentile). Body mass index is at the 85th percentile for age.
General: She is awake and alert, in mild respiratory distress. Head/eyes/ears/throat: Her conjunctiva and tympanic membranes (TMs) are normal. Her nasal mucosa is erythematous with yellowish discharge. There is mild maxillary sinus tenderness. Her lips and mucous membranes are moist. Tonsils are 1+, pharynx with mild erythema, no exudates noted. Tachycardia is present with regular rhythm and no murmurs noted.
Mild intercostal retractions are noted with decreased air entry over left lower lobe with fine crackles. No expiratory wheezes are auscultated. There is increased vocal fremitus over the left base with dullness to percussion. Exam of the abdomen reveals bowel sounds present; it is soft and nontender to palpation.
Her skin and neurologic examinations are unremarkable.
The physical exam should focus on the respiratory system. The clinician should assess for tachypnea, retractions (intercostal, subcostal, suprasternal), wheezing, nasal flaring, or grunting. Tachypnea is a significant, although at times subtle, clinical finding associated with lower airway illness. Durbin and Stille (2008) use the following criteria as key indicators of the presence of pneumonia in a pediatric patient: > 50 breaths/min at 2 to 12 months of age, > 40 breaths/min at 1 to 5 years, > 20 breaths/min for those older than 5 years, subtracting 10 if the child is febrile. They emphasize that tachypnea is the most sensitive and specific sign of pneumonia, found twice as frequently in children who have evidence of pneumonia on chest radiography as in those who have no such findings (Durbin & Stille, 2008).
“The most common signs of pneumonia detected by office-based clinicians are dullness to percussion, crackles, decreased breath sounds and bronchial breath sounds (louder than normal tubular breath sounds often accompanied by egophony)” (Durbin & Stille, 2008, p. 150). New onset wheezing is not typically associated with bacterial pneumonias (Durbin & Stille).
Making the Diagnosis
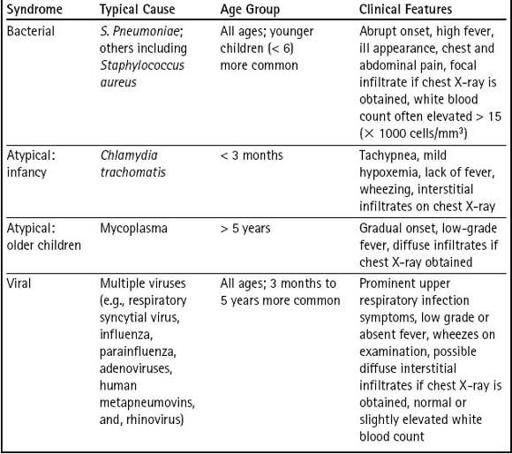
This history and physical examination are consistent with a diagnosis of pneumonia. There are three child and adolescent pneumonia syndromes: bacterial, atypical, and viral. (See
Table 24-2
.) Viruses are the most common etiology of pneumonia in older infants and children younger than 5 years of age. However, bacterial pathogens including
M. pneumoniae
and
C. pneumoniae
are most prevalent in school-age children (Gaston, 2002). Determination of the precise etiology of pneumonia is difficult due to a lack of sensitive and specific tests. Many clinicians treat pneumonia empirically with minimal laboratory or radiographic evaluation.
Do you need to do anything to confirm the diagnosis, such as a chest X-ray or laboratory studies?
In most instances, blood tests such as a complete blood count with differential (CBC), chemistries, or serology will not help to identify the cause of pneumonia or aid in the treatment. However, in a highly febrile child or infant
less than 3 months, a blood culture and CBC may be warranted (Brady, 2009). The white blood cell count is usually normal or mildly elevated with neutrophil predominance (Brady). When a more precise diagnosis is necessary, more invasive techniques are required. Bacteria found in blood, pleural fluid (thoracentesis), or lung tissue are considered diagnostic in a patient presumed to have pneumonia (Nohynek, Valkeila, Leinonen, & Eskola, 1995). Chest radiograph can be used to verify the clinical suspicion of pneumonia and characterize the disease process, but is not necessary for every patient.
Table 24–2 Common Clinical Pneumonia Syndromes
This child’s history and symptoms are typical of mycoplasmal pneumonia. Therefore, you decide that a chest radiograph is not needed at this time.
Management
Treatment must first be directed at whether the child needs to be admitted to the hospital or remain at home. The decision to hospitalize a child with pneumonia must be individualized and based upon age and several clinical factors. Typically, children who are less than 3 months old are hospitalized because they can deteriorate rapidly and are prone to hypoxemia and bacteremia (Durbin & Stille, 2008). A child of any age whose family cannot provide appropriate care and assure compliance with the therapeutic plan needs to be hospitalized. Other indications for hospitalization include:

