The Lupus Book: A Guide for Patients and Their Families, Third Edition (25 page)
Read The Lupus Book: A Guide for Patients and Their Families, Third Edition Online
Authors: Daniel J. Wallace

Again, this has no known clinical relevance.
Summing Up
Hormones are substances secreted by an endocrine gland in response to stimu-
lation by the brain. They are capable of modulating immunologic reactions, but
the extent to which this is clinically useful is not known except that female
hormones tend to promote immune responses, whereas male hormones are more
immunosuppressive. Nevertheless, male lupus is often more severe than female
lupus. Patients with SLE have an increased incidence of antibodies to glandular tissue and autoantibodies to reproductive organs, but the significance of this is not known. Sexual dysfunction is uncommon except that a few women with
SLE have disease-related vaginal dryness, vaginal sores, or arthritic hips.
The largest organ system in our body is the gastrointestinal (GI) tract. If it were laid out on a floor, the area from the throat to the anus would extend for 40
feet. So it should come as no surprise that such an important part of the body
can be involved in lupus. Actually, it is surprising that only limited portions of the gastrointestinal system are involved in the disease. This chapter will cover the relevant information for the lupus patient.
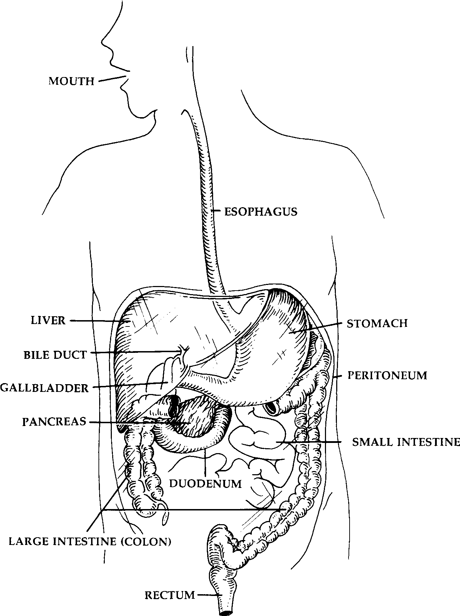
In addition, the GI system includes closely related regions that are not part
of the GI tract
per se
but either empty into it or have closely interrelated functions. These areas consist of the liver, pancreas, and biliary tree (bile ducts and gall bladder). In order to lend some order to this section, we will start at the top and work down. Figure 18.1 highlights the anatomy of the GI tract.
TAKE A GULP!
The upper GI tract begins in the throat and ends just beyond the stomach.
Starting from the top, persistent sore throats are common complaints of children with SLE, even though nothing is usually found on physical examination.
(Mouth sores are discussed in Chapter 12 and dental hygiene in Chapter 16.)
The oral cavity gives way to a long tube called the esophagus, which carries
food and liquid nourishment from the mouth, behind the chest cavity and heart,
and finally to the stomach. Esophageal problems in SLE are of two types: those
related to muscle dysfunction and symptoms related to reflux, or heartburn. The upper part of the esophagus wall contains a type of muscle called
striated
and the lower esophagus a type of muscle called
smooth
. The upper muscles are responsible for swallowing. Patients with certain other rheumatic diseases such as inflammatory myositis (dermatomyositis or polymyositis) have a high incidence of
dysphagia
, or difficulty swallowing. Interestingly, they seem to tolerate solid foods quite well, but liquids may come up through the nose and are some-
[134]
Where and How Can the Body Be Affected by Lupus?
Fig. 18.1.
Functional Anatomy of the GI Tract
times aspirated into the lungs. Approximately 10 percent of patients with lupus have a crossover (mixed connective tissue) disease with components of inflammatory myositis.
Barium swallows (a limited upper-GI x-ray procedure) or esophageal manom-
etry (which measures pressures) easily identifies the syndrome. About once a
year, I encounter an individual whose swallowing problem has posed such a
The Impact of Lupus upon the GI Tract and Liver
[135]
significant threat of aspiration pneumonia or malnutrition that I have one of my colleagues in head and neck surgery perform a procedure on the muscles known
as a cricopharyngectomy, which usually eliminates the problem.
WHY DO LUPUS PATIENTS GET HEARTBURN?
Phillip always had a sensitive stomach. When he started treatment for lupus,
his doctor prescribed Naprosyn, which relieved his joint pain but gave him
a mild gastritis. Phillip had a long-standing history of heartburn, which
worsened around the time he was diagnosed. An upper-GI x-ray series was
normal except for evidence of a hiatal hernia (fluid going back into the
esophagus from the stomach from displacement). He tolerated the gastritis
and didn’t tell anybody about it. Three months later, he attended a Bruins
football game. After an afternoon of fun and frolic which included eating
the end-zone pizza, consuming two Bruin dogs, and drinking three beers,
Phil began to feel as if he was digesting this haute cuisine again and again.
He thought that if he took an extra Naprosyn it might help his stomach
pain. The next morning he passed black, tarry stools and nearly passed out.
His family took him to an emergency room. When blood was drawn, he
was markedly anemic with a hemoglobin of 6. Dr. Gordon took him to
have an endoscopy (where doctors can visualize the stomach), where Phil
was diagnosed as having a hiatal hernia, erosive gastritis, and a duodenal
ulcer. Lucky to be alive, Phil was given a transfusion, started on Prilosec,
taken off Naprosyn, and given an appointment with the nutritionist.
Ten to 50 percent of lupus patients have problems with the esophagus, making
them painfully aware that this organ is not lined to protect itself from ‘‘acid rain.’’ Esophageal tissue is not equipped to handle acid, but stomach tissue is specially lined to handle this. The esophagus empties into the stomach, which
makes acid. There are a couple of reasons why fluid from the stomach ends up
back in the esophagus, or produces
reflux esophagitis
. It could be the way a person is built. The stomach may be higher than usual, and the sphincter (a
muscle) between the esophagus and stomach is weakened. This anatomic anom-
aly is a common finding in both healthy patients and particularly patients with lupus; it is called a
hiatal hernia
.
It could also be that your lower esophageal muscles may be incompetent and
fail to propel materials into your stomach correctly. Patients with crossover or mixed connective tissue disease have components of scleroderma and/or myositis and are especially predisposed to these problems. The net result of acidic stomach fluid entering the esophagus is not only heartburn but also scarring,
adhesions, and even poorer peristalsis (propulsion of the lower esophagus) from chronic ‘‘burns.’’
An upper-GI x-ray series is usually diagnostic. On occasion, an upper-GI
[136]
Where and How Can the Body Be Affected by Lupus?
endoscopy identifies additional problems, and at this procedure the esophagus
can be dilated, which may help to relieve symptoms. With heartburn, people
often automatically reach for antacids, which is a natural and understandable
reflex. But it’s only part of the solution. Esopahageal motility problems are
managed by eating small, frequent meals rather than a few large ones, and
patients are generally instructed not to lie down for at least 2 hours after eating.
Antacids, H antagonists (Tagamet, Zantac, Axid, Pepcid), motility agents (Re-
2
glan), sodium sulcrafate (Carafate), and especially proton-pump inhibitors (Nexium, Protonix, Acephex, Prilosec, Prevacid) are all effective to varying degrees.
INTERNALS AND EXTERNALS: NAUSEA, VOMITING,
DIARRHEA, AND CONSTIPATION
Anita experienced a change in her bowel habits. After a particularly stress-
ful experience at work, she began having diarrhea alternating with consti-
pation with mucousy stools. This was associated with bloating, cramping,
and distension. After a complete GI workup that ruled out other possibil-
ities, Dr. Berk diagnosed her as having functional bowel disease. Around
the same time, Anita’s internist told her that the muscle and joint aches she
complained about in her upper back and neck areas and which were keeping
her up at night were due to a closely related disorder known as fibro-
myalgia. Well-controlled on Levsin and a high-fiber diet, even Anita’s fi-
bromyalgia improved. Then she was diagnosed with SLE. Wondering
whether lupus had affected her intestines all along, Anita requested and her
doctor performed another evaluation which showed no evidence of lupus
activity in the GI tract. Dr. Berk diagnosed her as having a flareup of
functional bowel syndrome, which was resulting from generalized lupus
activity.
At various times, many of my patients complain of nausea, vomiting, diarrhea,
or constipation. The most common sources of these complaints are nonsteroidal
anti-inflammatory drugs (NSAIDs), corticosteroids, and chemotherapy. The rest
of the bowel complaints listed here are what doctors label
functional
. In other words, they represent a disorder that carries several names including
functional
bowel disease, spastic colitis, or irritable bowel syndrome
—all of which are related to abnormal intestinal motility or are due to malfunctioning of the autonomic nervous system. This condition correlates with the presence of fibro-
myalgia, which is not part of SLE. It is, however, seen in a large number of
lupus patients. Occasionally, the symptoms of nausea, vomiting, diarrhea, or
constipation reported by SLE patients are due to lupus or a concurrent inflam-
matory bowel disease such as ulcerative colitis.
The Impact of Lupus upon the GI Tract and Liver
[137]
PEPTIC ULCER DISEASE
Have you ever experienced a pain in the pit of your stomach that would not go
away? Until 1975, 20 percent of patients with SLE developed an ulcer during
the course of their disease. With the introduction of medications such as the H2
blockers (Tagamet, Zantac, Pepcid, Axid), sodium sucralfate (Carafate), proton-
pump inhibitors such as omeprazole (Prilosec), as well as an agent known as
misoprostol (Cytotec), the number of lupus patients with ulcers has decreased
to less than 5 percent. Though necessary to treat the disease, NSAIDs and cor-
ticosteroids can all produce erosions in the stomach or duodenum of the small
intestine, leading to ulcerations. Fortunately, selective cox-2 blocking NSAIDs (Bextra, Celebrex, Vioxx) and nonacetylated aspirin products (Disalcid, Trilisate) are much less likely to cause an ulcer than the older nonsteroidals. Gastric ulcers caused by the bacterium
Helicobacter pylori
may be more common in SLE and are treated with erythromycin-based antibiotics, ampicillin, bismuth
solutions, and proton-pump inhibitors.
IS INFLAMMATORY BOWEL DISEASE
ASSOCIATED WITH SLE?
Somewhere between 1 and 4 percent of lupus patients experience severe, crampy
abdominal pain with chronic diarrhea. They have developed a second autoim-
mune process known as
ulcerative colitis
. Characterized by inflammation of the superficial lining of the colon (large intestine), ulcerative colitis is treated with aspirin/sulfa antibiotic combinations (e.g., Azulfidine, Asacol) and, if necessary, steroids. Patients with lupus may have difficulty tolerating some sulfa derivatives.
Crohn’s disease
(or
regional ileitis
) and SLE are both autoimmune diseases, but curiously, very few patients are victims of both disorders. Since both are
autoimmune diseases, an increased concurrence with SLE would be anticipated.
In fact, lupus and Crohn’s disease have been reported together only a few times in the world’s literature.
WHAT IS ASCITES?
Some lupus patients notice a swelling in their belly and feel as though they
were pregnant. It has been estimated that at some point 10 percent of lupus
patients demonstrate
ascites
, a collection of fluid made by peritoneal tissue. The peritoneum is a thin membrane that lines the abdominal cavity, just as the pleura and pericardium line the lung and heart. We have already shown how pleurisy
and pericarditis develop as a result of irriation of these linings (Chapter 14).
[138]
Where and How Can the Body Be Affected by Lupus?
Peritonitis evolves similarly. Irritation of the peritoneum results in fluid formation (ascites) throughout the abdominal area. Ascitic fluid, like pleural fluid, is either a transudate or an exudate.
Transudates
(clear, sterile fluids) are painless and common when pleural or pericardial effusions are also present. Nephrotic syndrome, a condition observed when the kidney leaks protein, is also associated with ascites.
Exudates
can be painful and are thicker and cloudier, producing ascites when there is an infection, malignancy, pancreatitis, or serious inflammatory process in the abdomen. Usually identified at physical examination, ascites is also diagnosed by an ultrasound or computed tomography (CT) scan.
