The Rise and Fall of Modern Medicine (4 page)
Read The Rise and Fall of Modern Medicine Online
Authors: James Le Fanu

More than fifty years later this first description of the use of penicillin has lost none of its power to amaze. Reading it one has the impression of witnessing a miracle, whose origins, as is well known, lay in the chance observation made by Alexander Fleming in his laboratory at London's St Mary's Hospital over ten years earlier. As a microbiologist Fleming's research work involved growing colonies of bacteria on special plates called petri dishes and observing their behaviour in different circumstances.
He had, for example, recently shown that the chemical lysozyme, present in tears, could inhibit the growth of several types of harmless bacteria. But then in 1928, returning from his summer holidays, Fleming, picking up a petri dish standing in a pile waiting to be washed, noticed how a contaminating mould (later identified as
Penicillium notatum
) had inhibited the growth of a colony of staphylococcal bacteria that can cause many different types of infectious illness. He then extracted the juice from the mould (which he called penicillin) and showed it was capable of inhibiting the growth of a whole range of bacteria. Curiously, however, when other scientists tried to replicate the accidental method by which he had made his discovery, they were quite unable to do so.
It was not until 1964, almost forty years later, when Fleming's former assistant Ronald Hare investigated the matter in detail, that the reason emerged. Hare found that this failure to replicate Fleming's original observation was because the growth of the penicillium mould occurred at a different temperature (20 degrees Celsius) from that of the staphylococcus, which grows best at a temperature of around 35 degrees Celsius. So what had happened?
Firstly, the penicillium mould that had âfloated through the window' was not a commonly occurring strain but rather a rare one that had wafted up from the laboratory below, where a fellow scientist and fungus expert, C. J. LaTouche, was working. Fortuitously this rare strain just happened to produce large amounts of penicillin. Some spores, it must be presumed, contaminated a petri dish on which Fleming had been growing some colonies of staphylococci. Inexplicably, but essential for his subsequent discovery, Fleming did not, prior to going on holiday, place the dish in the incubator but left it out on the laboratory bench. Consulting the meteorological records for
London at the end of July 1928, Ronald Hare discovered that while Fleming was away there had been an exceptionally cool nine-day period â which would have favoured the growth of the penicillium mould â after which the temperature rose, which would have stimulated the growth of the staphylococcus. The penicillium mould was by now producing sufficient quantities of penicillin, and on his return Fleming noted that the pinhead-sized yellow spots on the plate, each of which represented a colony of the staphylococcus, had an unusual appearance. âFor some considerable distance around the mould growth the colonies were obviously undergoing lysis [dissolution].' Thus, without the ânine cool days' in London in the summer of 1928, Fleming would never have discovered penicillin.
3
Fleming was much luckier than he realised, but he was then remarkably indolent in exploring the therapeutic potential of his findings. He used juice extracted from the penicillium mould to cure a colleague suffering from the mild bacterial infection conjunctivitis, but by the following year he had abandoned any formal research into its further clinical use, because of the prevailing view that naturally occuring chemicals such as penicillin were likely to be too toxic to be used to treat infectious diseases.
4
Fleming did not take the matter further because he did not think it worth pursuing, âa good example of how preconceived ideas in medicine can stifle the imagination and impede progress'.
5
So the near miraculous properties of penicillin had to be rediscovered all over again ten years later by Howard Florey and Ernst Chain in Oxford, which was preceded, interestingly enough, by recapitulation of Fleming's work on the antibacterial properties of lysozymes in tears. Howard Florey had arrived in Britain from his home country of Australia in 1922, and after
graduating from Oxford rapidly ascended the academic ladder. He was prodigiously industrious, very good with his hands and had the knack of attracting others as, or more, talented than himself to work as his collaborators. In 1935 when still only thirty-seven he was appointed Professor of Pathology at Oxford and promptly recruited Ernst Chain, a young German Jewish chemist refugee from Nazi Germany. Florey's scientific interests included the study of the chemistry of the body's natural secretions, so he initially hoped that Chain's talents would be able to elucidate their biochemical structure. âWhen Florey and I in our first meeting discussed the future research programme in the department, Florey drew my attention to a very startling phenomenon,' Chain recalled. This was Fleming's observation, made back in 1921, that lysozymes in tears and nasal secretions were capable of dissolving thick suspensions of bacteria, though how they attacked the cell walls of bacteria was unknown. It took only a year for Chain to show that lysozyme was a complex enzyme. While writing up this work for publication, he looked around for other instances of compounds that might destroy bacteria and inevitably came across Fleming's original paper describing the effects of penicillin. By now it should be clear why Chain and Florey were to succeed where Fleming had failed. The skills of a microbiologist like Fleming lay in the observation and interpretation of experiments with bacteria; the skills of a biochemist like Chain lie at a deeper level, in identifying the biochemical mechanisms that underpin the microbiologist's observations. And so just as Chain had so rapidly solved the question of the biochemistry of lysozyme, it was only a matter of time before he would unravel the mechanisms of the action of penicillin and appreciate its real significance.
Nonetheless, at the outset neither Chain nor Florey believed
penicillin would have any âclinical applications' in the treatment of infectious diseases, so the precise sequence of events that persuaded them to change their minds is of some interest. Firstly it seems that Chain was intrigued to find that penicillin was âa very unusual substance'. It was not, as he had imagined it would be, an enzyme like lysozyme, but rather it turned out to be âa low molecular substance with great chemical instability'. In brief, he had no idea what it was, so âit was of obvious interest to continue the work'. Secondly, he had the biochemical skills to extract and purify (though not to a very great extent) penicillin, which when tested against bacteria grown in culture proved to be twenty times more potent than any other substance. Thirdly, when penicillin was injected into mice it was apparently ânon-toxic'. This last point was vital, for, as already pointed out, probably the most important reason why Fleming had failed to pursue the possibilities of penicillin was the common belief that any compound capable of destroying bacteria would necessarily harm the person to whom it was given. Finally, in a classic experiment Chain and Florey demonstrated that penicillin could cure infections in mice: ten mice infected with the bacterium streptococcus were divided into two groups, with five to be given penicillin and five to receive a placebo. The âplacebo' mice died, the âpenicillin' mice survived.
6
Florey naturally hoped the publication of the compelling results of the mice experiment in
The Lancet
would prompt interest from major pharmaceutical companies for, a man being 3,000 times larger than a mouse, it would require prodigious quantities of penicillin to assess its effects in humans. But these were difficult times. The previous year Britain had declared war on Germany and the British Expeditionary Force of 350,000 men had just been driven on to the beaches of Dunkirk to be
evacuated by an improvised armada of ships that somehow survived the repeated attacks of the German dive-bombers. This shattering defeat, in which Britain lost the equivalent of an entire army, made the prospect of a German invasion almost inevitable and heralded the Luftwaffe's daily assaults on London in the Battle of Britain.
At this desperate moment, when the future of Britain lay in the balance, Florey decided, astonishingly in retrospect, to commit the puny resources of his laboratory in Oxford to making enough penicillin to test in humans. âThe decision to turn an academic university department into a factory was a courageous one for which Florey took full responsibility . . . if his venture had failed it would have been seen as an outrageous misuse of property, staff, equipment and time, and Florey would have been severely censured.'
7
The hallmark of Florey's university-laboratory-turned-penicillin factory was improvisation, the penicillium moulds being grown on hospital bedpans and the precious fluid extracted and stored in milk jugs:
[In] the âpractical' classroom, the washed and sterilised bedpans were charged with medium and then inoculated with penicillin spores by spray guns. They were then wheeled on trolleys to what had been the students' âpreparation' room, now converted into a huge incubator kept at 24° Centigrade. After several days of growth, the penicillin-containing fluid was drawn off from beneath its mould by suction . . . The air was full of a mixture of fumes: amyl acetate, chloroform, ether. These dangerous liquids were pumped through temporary piping along corridors and up and down stairwells. There was a real danger to the health of everyone involved and a risk of fire or explosion that no one cared to contemplate.
8
By the beginning of 1941 there was just enough penicillin for the first trial in humans. On 12 February Charles Fletcher administered the first injection directly into the policeman Albert Alexander's vein, with the results just described. Seven university graduates, including two professors and ten technical assistants, had worked every day of the week and most nights for several months to achieve these results. In June Florey travelled to America, where eventually four major drug companies took up the challenge of the mass production of penicillin.
Come the end of the war, in 1945, Florey and Chain shared, along with Fleming, the Nobel Prize. Their achievement was not just the development of penicillin but rather the clarification of the principles by which
all
antibiotics were subsequently to be discovered. Florey, in his acceptance speech, spelled them out: first, the screening of microbes to identify those that produced an antibacterial substance; then, the determination of how to extract the substance; then testing it for toxicity and investigating its effect in animal experiments. And finally, tests in humans.
9
We now know, though Florey did not when he gave his speech, that penicillin was not just âa lucky break'. Rather the screening of tens of thousands of species of micro-organisms over the next few years revealed a handful that produced a whole further range of antibiotics (see page 23) whose profound impact on medicine has already been mentioned; but four further points are worth noting. It can be difficult to appreciate the comprehensiveness of the antibiotic revolution. There are many different types of infectious illness, from the trivial such as a sore throat to life-threatening meningitis. The bacteria involved behave in different ways, both in how they spread themselves around and how they damage the body's tissues. So, an attack of meningitis can kill within twelve hours
while tuberculosis may take ten years or more. And yet there is not one of the hundreds of different species of bacteria that cause disease in humans that is not treatable with one or other antibiotic.
Then, while the mechanism of action of antibiotic-producing bacteria might seem simple, their effects are both very diverse and highly complex. They can interfere with the enzymes that make the cell wall, blow holes in the lining of the cell, disturb the transport of chemicals across the lining, or inhibit the manufacture of proteins in the cell.
10
Next, the chemistry of antibiotic molecules is very unusual. It was hoped in the early days following the discovery of penicillin that the drug could be synthesised, thus avoiding the necessity of growing the penicillium mould in vast fermentation plants. But that was not to be, as one of those involved, John C. Sheehan, subsequently commented:
Behind the feat of elucidating the structure of penicillin lay the deceptively simple problem of understanding how one carbon atom is bound to one nitrogen atom. When these two atoms are properly connected this gives penicillin its antibiotic properties. When the carbon and nitrogen atoms do not connect, the penicillin compound is not penicillin. Thousands of chemists, biochemists, organic chemists, physical chemists, microbiologists, technicians and government bureaucrats struggled for years to make those atoms hook up with each other. Millions of dollars were spent from public and private treasuries. But despite the money and labour lavished on the problem, the enchanted ring of penicillin could not be mastered.
11
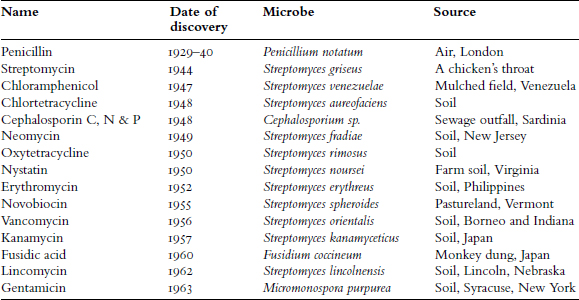
Dates of the discovery and sources of the more important antibiotics
12