Breast Imaging: A Core Review (7 page)
Read Breast Imaging: A Core Review Online
Authors: Biren A. Shah,Sabala Mandava
Tags: #Medical, #Radiology; Radiotherapy & Nuclear Medicine, #Radiology & Nuclear Medicine

Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:18.
8a
Answer A.
Repeat imaging is required due to chin artifact on MLO view. BI-RADS Assessment is 0.
8b
Answer C.
Repeat imaging is required due to chin artifact on MLO view.
Reference: Shah BA, Fundaro GM, Mandava S.
Breast Imaging Review: A Quick Guide to Essential Diagnoses
. 1st ed. New York, NY: Springer; 2010:2–5.
9
Answer E.
The posterior nipple line measurement difference between MLO and CC view should not exceed more than 1 cm if there is adequate tissue exposure.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:5–7.
10
Answer C.
Reference:
http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActand Program/Guidance/PolicyGuidanceHelpSystem/ucm135427.htm
11
Answer C.
Reference:
http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActand Program/Guidance/PolicyGuidanceHelpSystem/ucm052165.htm
12
Answer A.
Reference:
http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActand Program/Guidance/PolicyGuidanceHelpSystem/ucm052779.htm
13a
Answer A.
Repeat MLO view is needed due to high-density particles seen in the axillary region that may represent deodorant artifact.

13b
Answer D.
Images show no high-density particles in the axillary region, which proves the findings seen previously were deodorant artifact.
Reference: Shah BA, Fundaro GM, Mandava S.
Breast Imaging Review: A Quick Guide to Essential Diagnoses
. 1st ed. Springer; 2010:2–5.
14
Answer E.
Asymptomatic women 40 years of age or older should have an annual screening mammogram. It is unclear at what age, if any, women cease to benefit from screening mammography. Because this age is likely to vary depending on the individual’s overall health, the decision as to when to stop routine mammography screening should be made on an individual basis by each woman and her physician.
Reference: American College of Radiology (ACR).
ACR Practice Guidelines for the Performance of Screening and Diagnostic Mammography
. American College of Radiology; May 2013,
http://amclc.acr.org/LinkClick.aspx?fileticket=dQDASxSIrJ4%3D&tabid=61
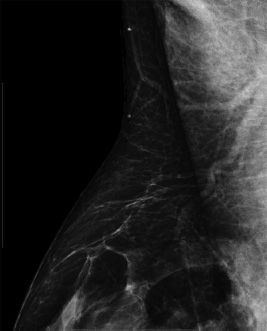
15
Answer E.
The nipple should be in profile on at least one view. This may require an extra view in addition to the typical CC and MLO views.
A.
The MLO view is a projection parallel to the pectoralis major muscle.
B.
On the CC view, the pectoralis major muscle is seen approximately 30%–40% of the time.
C.
On the MLO view, the pectoralis major should be convex anteriorly—never concave.
D.
On the MLO view, the pectoralis major muscle should be seen to or below the level of the axis of the nipple.
References: Brant WE, Helms CA.
Fundamentals of Diagnostic Radiology
. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:569–570.
Cardenosa G.
Breast Imaging Companion
. 3rd ed. Philadelphia, PA: Lippincott Williams & Willkins; 2008:79–88.
16
Answer D.
Reference:
http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActand Program/Guidance/PolicyGuidanceHelpSystem/ucm135449.htm
17
Answer C.
Reference:
http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActand Program/FacilityScorecard/ucm113812.htm
18
Answer A.
The U.S. Congress appointed the Food and Drug Administration (FDA) to develop guidelines to oversee the quality of mammography equipment and facilities after the enactment of the Mammography Quality Standards Act (MQSA) in 1992. Various states have also been certified to accredit mammography facilities; these are approved by the FDA.
References: Kopans DB.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:267–268.
Radiation-Emitting Products.
www.fda.gov/radiation-emittingproducts/mammographyqualitystanda rdsactand program/default.htm
19
Answer B.
Ghosting from cardiac or respiratory motion occurs in the phase-encoding direction. It can be prevented from obscuring breast tissue by proper selection of phase- and frequency-encoding directions. Patient motion causes blurring of the poor shimming results in poor fat suppression.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:197.
20
Answer C.
Reference: ACR BI-RADS—Mammography.
ACR Breast Imaging Reporting and Data System, Breast Imaging Atlas
. 4th ed. Reston, VA: American College of Radiology; 2003:230.
21
Answer B.
BRCA-1 is autosomal dominant and is a tumor suppressor gene on chromosome 17. BRCA-2 is on chromosome 13. The lifetime risk of breast cancer is 50% to 85%. It is associated with an increased risk of ovarian cancer and other cancers such as prostate cancer. There is no known increased risk of lung cancer.
Reference: Berg WA, Birdwell RL, Gombos EC, et al.
Diagnostic Imaging Breast
. 1st ed. Salt Lake City, UT: Amirsys; 2006:Chapter 2, 25–26.
22
Answer C.
The current benchmark for CDR is 2–10/1000. It is expected with the BI-RADS 5th edition, that this will be changed to >2.5/1000.
Reference:
The ACR Breast Imaging Reporting and Data System (BI-RADS). BI-RADS—Mammography
. Reston, VA: American College of Radiology; 2003:234.
23
Answer A.
Reference: The
ACR Breast Imaging Reporting and Data System (BI-RADS). BI-RADS—Mammography
. Reston, VA: American College of Radiology; 2003:9–52, 234.
24
Answer B.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:16.
25
Answer D.
The difference between the line from the nipple to the pectoralis muscle on MLO and the line from the nipple to the back of the film on CC is 1 cm.
Good quality control for a properly positioned breast is essential for maximum tissue evaluation on a screening mammogram. The CC projection should complement the MLO projection, and the breasts should be positioned symmetrically to one another. It has been established that the proper positioning of the CC and MLO projections is determined by the difference in distance between the nipple to the pectoralis muscle on the MLO view (NL-MLO) and nipple to the back of the film on CC (NL-CC) is ≤ 1 cm. In other words, NL-MLO minus NL-CC is ≤ 1 cm. The pectoralis muscle can be seen in an estimate of 30% of the CC views.
References: Bassett LW, Hirbawi IA, DeBruhl N, et al. Mammographic positioning: Evaluation from the view box.
Radiology
1993;188:803–806.
Kopans DB.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007: 297–298.
26
Answer E.
Mammography compression plate and imaging receptor needs both 18 × 24 cm and 24 × 30 cm size, with compression force 25 to 45 pounds, with a moving grid for each image receptor size, and the collimation to the receptor while not the breast contour.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:5.
27
Answer D.
This artifact is caused by saturation of silicone signal, which can occur when silicone is selected for saturation rather than fat. Fat and silicone resonate closely at 1.5 T. Note that silicone was saturated in this image, but fat was not correctly saturated. As a result of silicone saturation, a silicone breast implant will have dark signal and the examination will be rendered nondiagnostic for evaluation of implant rupture. The inversion recovery (IR) sequence with water saturation is a silicone-specific sequence (water and fat will be saturated) that is the most important sequence of the examination. Silicone should appear white on this sequence, enabling the detection of intracapsular and/or extracapsular rupture. Answer A is wrong because susceptibility artifact is a signal void or field inhomogeneity caused by metal in or on the patient’s body. Answer B is wrong because wrap or aliasing artifact occurs when tissue extends beyond the field of view (FOV), causing signal from tissues outside the FOV to be superimposed on structures within the FOV. It occurs in the phase encoding direction. This artifact can be seen with patients’ arms in breast MRI practice. Answer C is not correct because RF interference is an artifact that occurs due to incomplete shielding of the MRI suite (e.g., door ajar) or radiofrequency disturbance within the MR suite (e.g., patient monitoring equipment). This artifact manifests as repetitive lines extending across the image at a fixed interval.
Reference: Hendrick RE.
Breast MRI: Fundamentals and Technical Aspects
. New York, NY: Springer; 2008:187–207.
28a
Answer D.
Abnormal interpretation rate, also known as recall rate, in screening mammography is the percentage of examinations interpreted as positive. For screening mammography, positive exams include BI-RADS category 0, 4, and 5 assessments given based on screening mammograms.
Screening abnormal interpretation rate = (Category 0, 4, and 5 cases based on screening mammograms)/(Total number of screening mammograms) = 400 + 0 + 0/5,000 = 400/5,000 = 0.08 = 8%.
For diagnostic mammography, abnormal interpretation rate or biopsy recommended rate is the percentage of examinations interpreted as positive. For diagnostic mammography, positive exams include BI-RADS category 4 and 5 assessments based on diagnostic workup.
Other books
Costa 08 - City of Fear by Hewson, David
Bound by Her Best Friend (A Club Smex Story) by Shortt, Emma
Seducing Anne by Chanse Lowell, Marti Lynch, Shenani Whatagans
Betrayal: Abby's Guilt (The Betrayal Series) by Velardi, Sofia
The Alchemist’s Code by Martin Rua
Backstage Pass by Ryan, Nicole
Picture Perfect Wedding by Fiona Lowe
Button, Button: Uncanny Stories by Richard Matheson
Wherever You Are by Sharon Cullen
The New Year Dragon Dilemma by Ron Roy
