Digestive Wellness: Strengthen the Immune System and Prevent Disease Through Healthy Digestion, Fourth Edition (19 page)
Authors: Elizabeth Lipski

Cooked, packaged, or processed foods are enzyme depleted. Cooking at temperatures as low as 118 degrees Fahrenheit destroys enzymes. Since these kinds of foods are what we eat, most of us will benefit from enzyme supplementation.
Studies reveal that about 10 percent of 10-year-olds have enzyme deficiencies, 20 percent of 20-year-olds have enzyme deficiencies, 50 percent of 50-year-olds have enzyme deficiencies, and so on. This can occur from stress or low-grade inflammation in the stomach, called gastritis, and infections, such as H. pylori.
Enzyme deficiencies are obvious in children with cystic fibrosis, but less obvious as a pivotal factor in type 2 diabetes and obesity in our children. Enzyme supplementation has been helpful in the treatment of these health problems.
Supplemental enzymes have also been used successfully to treat several types of arthritis in adults, working more effectively than drug treatment. Moreover, they have been used successfully to treat children and adults with food allergies, eosinophilic gastroenteritis, asthma, and other illnesses. Along with probiotics, they are the first thing I think of when working with children and adults who are failing to
thrive. Other diseases that enzymes have been used clinically for include Crohn’s disease, ulcerative colitis, hay fever, pulmonary fibrosis, sinusitis, multiple sclerosis, bladder infections, and in breaking up and preventing blood clots. The effect on blood clots also protects us from heart disease.
Protein-splitting enzymes are used to reduce swelling and pain throughout the body and can be used to treat injuries. In one study, soccer players were given enzymes or placebos after they were injured. Injuries healed more quickly when enzymes were given, sometimes up to twice as fast. They can be used to reduce the time that bruises take to heal by about 50 percent.
Enzymes have also been used for decades in cancer treatment, especially in Europe. I recently heard oncologist Dr. Mahesh Kanojia speak at a medical conference. He said that use of Aspergillus-derived protein splitting, also called proteolytic enzymes, enzyme supplements lessens the side effects of chemotherapy, including hair loss, and enhances the results of the treatments. Nicholas Gonzales, M.D., in New York, uses pancreatic enzyme supplements as a critical part of his individualized programs for people with all types of cancers. The National Institutes of Health (NIH) was so impressed, they funded a study to reproduce his work. This study did not show effectiveness of Dr. Gonzales’s treatments, but he has contested the way in which the evaluation was performed.
According to Dr. Brad Rachman, proteolytic enzymes improve protein digestion and decrease the quantity of antigens that leak into the bloodstream. This can reduce issues with food allergies and food sensitivities.
There are three major types of supplemental enzyme products: pancreatic enzymes, enzymes grown on a fungal base, and plant-based enzymes.
Pancreatic enzymes have been used and are part of common medical practice for illnesses such as cystic fibrosis. They are actually derived from animal pancreatic tissue. They work well to assist with digestion and to help stabilize blood glucose levels in people with diabetes and hypoglycemia. When I was in my 20s I suffered from hypoglycemia; I took pancreatic enzymes several times a day for about a year and found my hypoglycemia to be nearly 100 percent gone. The difficulty with pancreatic enzymes is that they work in a limited pH range, at 8 or above. This pH is too alkaline to function in the stomach, where a large part of digestion takes place. In cystic fibrosis a small percentage of children become allergic to pancreatic enzymes.
More recently, enzymes have been grown on a fungal base of Aspergillus niger and Aspergillus oryzae. New to the United States, these enzymes have been used in food production for centuries and clinically for more than 50 years in Japan. There
are hundreds of species of Aspergillus, but these two have been found to be completely free of mycotoxins (substances produced from fungi that are toxic). These enzymes are blended like wine to ensure that they work in the high acid environment of the stomach and through the small and large intestines, which have a more neutral pH. They also are not derived from an animal protein and have been found to cause fewer allergic issues in people.
Plant-based enzymes, such as bromelain and papain, are protein-splitting enzymes. Bromelain is derived from the green stems of pineapple plants, and papain comes from green papayas. They are useful for reducing inflammation and pain and for digestion of protein.
Enzymes are rated by their activity level rather than by counting milligrams or micrograms of them. When you purchase enzyme supplement products, you will see units such as DU, HUT, FCCLU, CU, IAU, and many others to express the level of enzyme activity. If you look at an enzyme label and it measures the enzymes only in milligrams or micrograms, you cannot know if there are any active enzymes in the product at all. Enzyme supplements are very stable and will last for at least three years, so many labels do not have expiration dates.
Insufficient dietary fiber intake is yet another reason people may not be absorbing or digesting their foods appropriately. In fact, most of us eat half as much fiber as our ancestors did. Soluble fiber (found in fruit, beans, barley, rice, flaxseed, and psyllium) helps bind bile acids, regulates cholesterol and blood sugar levels, and keeps our intestinal pH in balance. Insoluble fiber (found in bran, vegetables, whole grains, and carrots) helps keep us regular and normalizes peristalsis. Insoluble fiber is fermented in our large intestines by beneficial bifidobacteria to produce butyrate and other short-chain fats that provide fuel and cell maintenance in our large intestines. Soluble fiber helps to regulate both constipation-type and diarrhea-type irritable bowel syndrome. Improvement in bowel function may help prevent diverticulosis, appendicitis, colon polyps, colon cancer, hemorrhoids, and varicose veins. Diets high in soluble fiber are helpful to people with irritable bowel syndrome, Crohn’s disease, hiatal hernia, and peptic ulcer. Dietary fiber also helps prevent obesity by slowing down digestion and the release of glucose and insulin. Fiber has been shown to normalize serum cholesterol levels. High-fiber diets reduce the risk of heart disease, high blood pressure, and certain types of cancer. See
Chapter 12
for more information on increasing high-fiber foods in your diet.
4
Intestinal Permeability/Leaky Membranes
The foot bone connected to the leg bone,
The leg bone connected to the knee bone,
The knee bone connected to the thigh bone,
The thigh bone connected to the back bone,
The back bone connected to the neck bone,
The neck bone connected to the head bone
—African American spiritual/children’s song
Leaky gut syndrome
is really a nickname for the more formal term
increased intestinal permeability
, which underlies an enormous variety of illnesses and symptoms. It’s not a disease or an illness itself. It’s a symptom of inflammation and imbalance that has many causes. The list of health conditions associated with increased intestinal permeability grows each year as we increase our knowledge of the synergy between digestion and the immune system. Currently there are more than 8,000 research articles on intestinal permeability.
The small intestines have a paradoxical function. It allows only properly digested fats, proteins, and starches to pass through so they can be assimilated, while providing a barrier to keep out bacterial products, foreign substances, and large undigested molecules. This is called the barrier function of the gastrointestinal mucosal lining. This surface is often called the brush border because under a microscope its villi and microvilli look like bristles on a brush.
In between cells are junctions called desmosomes. Normally, desmosomes form tight junctions and do not permit large molecules to pass through. When the area is irritated and inflamed, however, these junctions loosen up, allowing larger molecules to pass through. The substances that pass through the intracellular junctions are seen by our immune system as foreign, stimulating an antibody reaction. When
the intestinal lining is damaged, larger substances of particle size are allowed to pass directly, again triggering an antibody reaction. (See
Figure 4.1
.)
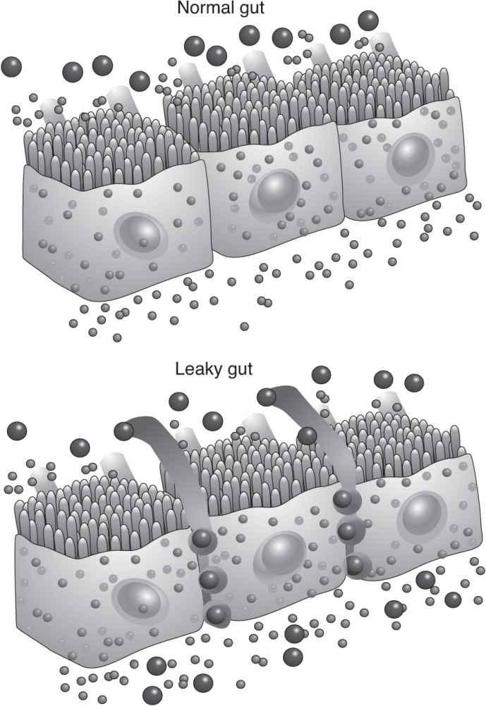
Figure 4.1
Leaky gut syndrome.
(Used with permission from Genova Diagnostic Laboratory.)
When the intestinal lining is damaged even more, substances larger than particle size—disease-causing bacteria, fungi, potentially toxic molecules, and undigested food particles—are allowed to pass directly through the weakened cell membranes. They go directly into the bloodstream, activating antibodies and alarm substances called cytokines. The cytokines alert our lymphocytes (white blood cells) to battle the particles. Oxidants are produced in the battle, causing irritation and inflammation far from the digestive system. Inflammation on this brush border can prevent small nutrients and food molecules from passing into the gut lumen. This is the primary cause of malabsorption.
Intestinal mucus normally blocks bacteria from moving to other parts of the body. But when the cells are leaking, bacteria can pass into the bloodstream and travel throughout the body. When intestinal bacteria colonize in other parts of the body, we call it bacterial translocation, and it is often found in people with leaky gut syndrome. For example, Blastocystis hominis, a bacteria that causes GI problems, has been found in the synovial fluid in the knee of an arthritis patient. Surgery or tube feeding in hospitals can also cause bacterial translocation.
Here’s how leaky gut syndrome works. Imagine that your cells need a kernel of corn. They are screaming out, “Hey, send me a kernel of corn.” The bloodstream replies, “I have a can of corn, but I don’t have a can opener.” So the can goes around and around while the cells starve for corn. Finally, our immune system reacts by making antibodies against the can of corn, treating the corn as if it were a foreign invader. Your immune system has mobilized to finish the job of incomplete digestion, but this puts unneeded stress on it. The next time you eat corn, your body already has antibodies to react against it, which triggers the immune system, and so on. As time goes on, people with leaky gut syndrome tend to become more and more sensitive to a wider variety of foods and environmental contaminants.
Depending on our own susceptibilities, we may develop a wide variety of signs, symptoms, and health problems. Leaky gut syndrome is associated with the following medical problems: allergies, celiac disease, Crohn’s disease, HIV, and mal-absorption syndromes. It is also linked to autoimmune diseases such as AIDS, ankylosing spondylitis, asthma, atopy, bronchitis, eczema, food and environmental sensitivities, other allergic disorders, psoriasis, Reiter’s syndrome, rheumatoid arthritis, Sjögren’s syndrome, and skin irritations.
The listed conditions can arise from a variety of causes, but leaky gut syndrome may underlie more classic diagnoses. If you have any of the common symptoms or disorders associated with leaky gut syndrome, ask your physician to order an intestinal permeability test to see if it is causing your problem. In addition to clinical conditions, people with leaky gut syndrome display a wide variety of symptoms.
Leaky gut syndrome puts an extra burden on the liver. All foods pass directly from the bloodstream through the liver for filtration. The liver “humanizes” the food and either lets it pass or changes it, breaking down or storing all toxic or foreign substances. Water-soluble toxins are easily excreted, but the breakdown of fat-soluble toxins is a two-stage process that requires more energy. When the liver is bombarded by inflammatory irritants from incomplete digestion, it has less energy to neutralize chemical substances. When overwhelmed, it stores these toxins in fat cells, much the same way that we put boxes in the garage or basement to deal
with at a later date. If the liver has time later, it can deal with the stored toxins, but most commonly it is busy dealing with what is newly coming in and never catches up. These toxins provide a continued source of inflammation to the body. Increased intestinal permeability has been found to be a factor in liver diseases, such as cirrhosis.
 CLINICAL CLUES ASSOCIATED WITH LEAKY GUT SYNDROME
CLINICAL CLUES ASSOCIATED WITH LEAKY GUT SYNDROME
