Flow: The Cultural Story of Menstruation (28 page)
Read Flow: The Cultural Story of Menstruation Online
Authors: Elissa Stein,Susan Kim
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #History, #Historical Study & Educational Resources, #Politics & Social Sciences, #Women's Studies, #Personal Health, #Social History, #Women in History, #Professional & Technical, #Medical eBooks, #Basic Science, #Physiology

Believe it or not, a normal, healthy woman doesn’t need a whole lot of extra iron to replace what she loses during menstruation; as a matter of fact, 90 percent is automatically replenished by one’s body. Nevertheless, women do regularly lose twice as much iron as do men, and therefore, a passing nod to replacing it is in order. Some find iron supplements a tad binding, so dietary iron is always a worthwhile alternative. Good sources are meat, poultry, and fish if one eats such things and green, leafy vegetables, enriched grains, and dried fruits if one doesn’t. And since iron absorption seems to be influenced by other dietary factors, it always helps to eat a balanced diet, especially one that contains a lot of vitamin C.
Overwhelmingly, the single most common menstrual problem women suffer from is endometriosis, a disease that is both caused and aggravated by menstruation (although postmenopausal women suffer from it, as well). Here’s the deal: in a healthy woman, endometrial tissue is found only in the uterus. Occasionally, however, tiny bits of endometrial tissue or clumps of cells can be carried out of the uterus and into the pelvic cavity by one’s menstrual flow.
Endometriosis is much more likely to occur in women who have never been pregnant, and has thus been named “the career woman’s disease.”
This isn’t such a big deal on its own, and in most cases, a woman’s immune system is able to handily dispose of any stray cells floating around. For others, however, should any of those fragments or cells come into contact with scarred or injured tissue, woe is you! They will happily attach themselves to their new home and immediately commence to reproduce. Those little devils can set up shop on the diaphragm, fallopian tubes, ovaries, bladder, or intestines, or inside the abdominal cavity. These endometrial colonies grow and grow, and as they respond to the hormonal cycle, they continue to act as if they were still in the uterus, doing what they’re programmed to do: thickening and building up when exposed to estrogen, then bleeding when estrogen levels drop. This cycle eventually causes scarring wherever the colonies have landed, as well as the formation of cysts. Since it’s a progressive disease, it ultimately leads to chronic discomfort, backache, nausea, and pain during sex and/or bowel movements. If left untreated, it can cause infertility in 30 to 40 percent of its victims and is one of the leading causes of childlessness worldwide.
More than 150 million women suffer from endometriosis worldwide, whether they’re aware of it or not … and if you have a mother or sister with endometriosis, your risk is seven times greater. It’s also much more likely to occur in women who have never been pregnant, and has thus been nicknamed “the career woman’s disease.” Ironically, the upswing in cases in the past few decades may well be due to social progress: as more women postpone maternity until their late twenties and early thirties, they’re more vulnerable to this painful and often dangerous condition.
So what’s a woman to do if she suffers from endometriosis? Or, for that matter, from severe dysmenorrhea, or fibroids? What are you supposed to do if your periods are genuinely screwing up your life?
Theoretically, one solution would be to just stay pregnant for the rest of your life, since pregnancy is a natural ovulation suppressant. So is breast-feeding, at least for a short while. During breast-feeding, one’s body produces prolactin while inhibiting the release of gonadotrophin, which in turn blocks ovulation and menstruation. Unfortunately, as birth control, this method is at best 98 percent effective, and only for the those first few months after giving birth.
The two most common ways to treat severe menstrual problems are through drugs or medical procedures. Every woman has to weigh her options carefully, because what works for her may be totally unacceptable to another. Any course of treatment she wants to undertake will have to be one based not only on her doctor’s diagnosis, the severity of the symptoms, and the possible risks of therapy, but on her own needs and concerns, as well.
There are chemical means of suppressing menstruation. These are generally contraceptives, synthetic hormones that can be administered orally, vaginally, via implant, or by injection. Taken regularly, they will regulate, reduce, or even eliminate one’s menstrual flow altogether, and also bring marked relief to anyone suffering from regular, severe pain. While there appear to be health benefits associated with long-term hormone use, there are also notable risks, especially for women who are over thirty-five, smoke cigarettes, and/or are overweight.
To treat endometriosis surgically, a woman can opt for varying degrees of just how radical an approach she finds acceptable. She can get a D&C, but if it’s not performed correctly, the procedure can result in infection, uterine perforation, or even infertility. Alternatively, a doctor can remove only the endometrial implants and leave everything else alone. Another option is for the entire endometrium to be cauterized, in a procedure called endometrial resection or ablation. These methods are considered fairly conservative, surgically speaking, although there’s a possibility that the endometrium or the implants could grow back. And like all medical procedures, there are always risks and possible complications that should be weighed seriously.
Myomectomy, in which the fibroids are removed hysteroscopically, through a tube, isn’t even considered surgery and can be done in a doctor’s office. One’s doctor, however, may argue against it, since it does take a certain amount of skill and experience; it definitely pays to find out how many he or she has performed to date. One will also probably be told that her fibroids could grow back. This, however, isn’t necessarily the worst-case scenario; even if a woman tends to grow fibroids like dandelions in the springtime, most don’t cause any problems at all.
The most radical way to stop menstruation and all of its problems is via hysterectomy, i.e., the surgical removal of the uterus. The removal of the ovaries is called an oophorectomy, and the two procedures are often performed together.
The first recorded hysterectomy was done in ancient Greece, in A.D. 100, and it was performed through the vagina. As doctors since time immemorial believed that the uterus was the seat of everything wrong with a woman, untold millions of healthy organs have been removed over the centuries, regardless of any proof that the operation did anything other than kill a whole lot of women; by the late 1880s, there was a 50 percent death rate for the procedure.
And what are the effects of hysterectomy, anyway? To us, they seem wildly contradictory. Regarding sex, for instance, some women report the loss of pleasurable uterine contractions during orgasm, diminished lubrication, and pain caused by scar tissue in the vagina. Yet other women are delighted by the freedom from uterine cramps and pain, as well as the relief of never having to worry about getting pregnant again. For them, having a hysterectomy is a shot in the arm and a huge boost to their sex lives. Some women suffer from depression after having the uterus removed, whereas others report being much happier. Some women (virtually all heterosexual) worry that their femininity and allure have diminished after their hysterectomy; still others feel an upsurge in confidence.
These, clearly, are intensely personal reactions that are hard to predict. After all, who can really say how anyone would react to the surgical removal of an organ, especially one so closely tied to our gender as the good old uterus?
Moreover, there are also significant physical complications worth weighing if one is seriously contemplating a hysterectomy. After all, it is major abdominal surgery, with all of the usual risks (adhesions, lesions, intestinal blockage, thrombosis). There are other possible complications worth weighing, as well. Even if one has opted to keep one’s ovaries, for example, they occasionally end up inert. Furthermore, the sudden absence of the prostaglandins normally produced by the uterus may increase one’s risk of heart disease and high blood pressure.
Scarily enough, some women don’t realize until too late that what they thought was a plain old hysterectomy also involved an oophorectomy, as well … and that the surgical removal of their ovaries brings on a sudden drop in hormones that can bring about other problems. Such possible side effects may include arthritis, osteoporosis, chronic fatigue, greater susceptibility to heart disease, depression, and mood disorders. Oophorectomy before menopause can also put a woman at greater risk for dementia and Parkinson’s disease. And who needs that, we ask?
For virtually all of history, the uterus has been pretty much thought of as either a wandering kind of animal, a passive sack that a baby grew in once in a while, or the seat of a woman’s emotions. But in fact, we now know it produces hormones, proteins, and sugars, not to mention prostaglandins that help our vascular tone and possibly help keep our circulatory system in good health. The uterus is also a crazy drug factory, making and secreting huge amounts of natural opiates that are closely related to marijuana, heroin, and morphine (we’d probably all be in prison if anyone in the White House knew). It’s an extraordinarily complex organ, as mysterious as the bottom of the sea, that clearly has a dynamic yet still unknown relationship with the rest of the body … and it’s not something to be snipped out and disposed of lightly.
And yet the United States is currently one of the world’s leaders in the procedure; every year, more than 600,000 women have a hysterectomy, making it the second most commonly performed surgery in the country. (Hey, and do you know what the first most commonly performed procedure is? A hint: it involves the same organ, the only organ, in fact, that doesn’t have an analogous equivalent in the male anatomy. Answer: the cesarean section.)
This translates to the fact that the uterus of at least one out of three American women, mostly between the ages of twenty and forty-nine, will be surgically removed, and often the ovaries and cervix, as well. Overwhelmingly, the surgery is performed for noncancerous problems: fibroids, endometriosis, benign growths, uterine prolapse, menorrhagia. Disturbingly, there are some weird discrepancies in who gets the procedure and who doesn’t. Rates are twice as high in the South as they are in the Northeast, and higher in rural areas than in cities. African-American women in their early forties have the highest hysterectomy rate of all. And what’s most disturbing is that some researchers believe that at least a third of all hysterectomies are medically unnecessary.
THE COST OF BEING FEMALE
Have you ever wondered, as did wild-eyed feminists in the 1970s, if there’s something wrong about our even having to pay for femcare products in the first place? Gloria Steinem once quipped, “If men could menstruate … sanitary supplies would be federally funded and free,” just like the toilet paper and soap in any public restroom. And why is it that in many states in the United States, not to mention countries like Canada and Australia, tampons and pads aren’t considered “nonluxury” items, i.e., essential, and are thus subject to sales tax? Do you really consider that monthly packet of plugs a luxury?
As we’ve said before, we know that menstruation is one of our most personal processes and that the perception of pain is wildly subjective. Medical and surgical solutions to menstrual problems have unquestionably helped untold numbers of women live happier, fuller lives; what’s more, we fully support any female’s right to control her own body.
That being said—we’re still fans of the uterus. What can we say? As Natalie Angier pointed out so eloquently in her book Woman: An Intimate Geography, “To make a truly informed choice, we need information.” If you’re being driven to despair by menstruation, get all the facts you can and thinktwice.
And then sleep on your decision and thinkagain.
HEY, IS IT GETTING HOT IN HERE?
W
OULD YOU EVER PAY MONEY TO SWALLOW horse urine?
Okay … that’s kind of a disgusting question to ask out of the blue, and we’re sorry we just sort of sprang it on you. That being said, we feel compelled to ask this because, believe it or not, one of the bestselling prescription meds of all time is created using that selfsame liquid.
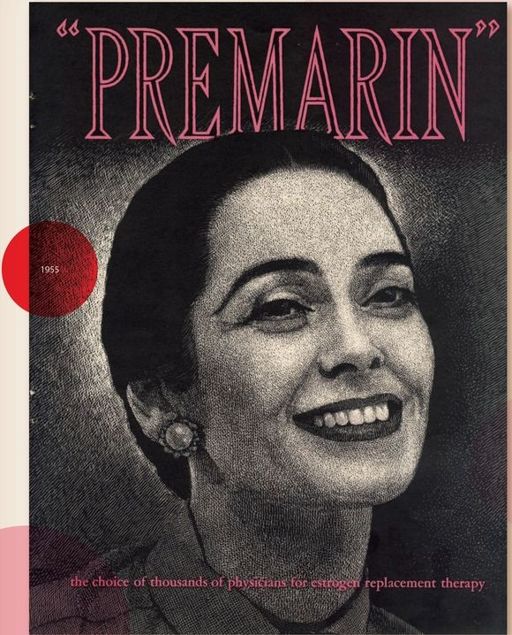
Premarin—introduced by Wyeth-Ayerst in 1943 to alleviate symptoms of menopause—is a synthetic estrogen product extracted from pregnant mares’ urine (PMU). Currently, more than nine million women in the United States take it for estrogen replacement therapy; according to the Humane Society of the United States, it takes about fifty thousand not-very-well-treated horses kept pregnant as continuously as possible on more than five hundred “PMU farms.” The foals are prematurely weaned and a lucky few are auctioned off to private owners. The rest are fattened up at feedlots until they’re big enough to be slaughtered for their meat. And all this is just to keep the labs stocked with enough pregnant mares’ urine to meet the increasing demand.
Wyeth
Pardon us …but blechh.
