Flow: The Cultural Story of Menstruation (30 page)
Read Flow: The Cultural Story of Menstruation Online
Authors: Elissa Stein,Susan Kim
Tags: #Health; Fitness & Dieting, #Women's Health, #General, #History, #Historical Study & Educational Resources, #Politics & Social Sciences, #Women's Studies, #Personal Health, #Social History, #Women in History, #Professional & Technical, #Medical eBooks, #Basic Science, #Physiology

[Hot flashes are] vicious, evil, all-consuming, demanding, unpredictable, hitting anywhere, anytime. When I am at home, I run to the fridge and stand in front of the freezer—I started wearing tanks so I could strip wherever I was. I hope those furnace-like outbursts of hormonal upheaval will never, never return.
—Carla S. (51)
may feel as if a severe panic attack is coming on, as her body is swamped in heat and she slowly starts to asphyxiate. The entire experience can be negligible, humiliating, nothing much, debilitating, mildly amusing, or horrifying.
Some women get a funny feeling, an aura or premonition that a hot flash is headed their way and can at least steel themselves for the inevitable; others just get blindsided by that wall of heat. While hot flashes seem to come out of nowhere, eating hot or spicy food, drinking alcohol or caffeine, or being stressed out can all be triggers. When they happen at night, they’re
The worst of it are the night sweats! Covers on, covers off, legs in, legs out, clothes on, clothes off. I have not had a full eight hours of sleep in I don’t know how long.
—Gerry C. (49)
called night sweats and can make one’s normal sleep patterns totally wack, even leading to sleep deprivation. It’s been reported that up to 75 percent of women experience night sweats at some point.
And yet menstrual disruptions and hot flashes are just two stars in the large cast of perimenopausal symptoms. Women routinely experience mood swings, spaciness, tearfulness, mental fogginess, and forgetfulness, making it a Herculean challenge to realize that the keys one has misplaced are actually in one’s hand. There’s often unexpected weight gain, and invariably in the last places one wants it, namely the hips, waist, and abdomen (although sometimes the breasts, as well). Speaking of breasts, they can often feel achey and tender to the point of actual pain.
That memory-loss thing is killing me … . I was a sharp person all my life and remembered most details, and now I don’t remember anything.
—Samantha W.(55)
In addition, perimenopausal women may experience insomnia, dizziness, vertigo and/or migraines, heart palpitations, dry skin, hair loss, and urinary incontinence.
Another area of great concern to many, as well as to their partners, is sex. As they approach menopause, many women feel their libidos evaporate like morning dew on a hot day, whereas others feel an unprecedented surge of randiness. But regardless of interest level, thinning of the vaginal walls and less lubrication can make intercourse uncomfortable, even painful.
So here’s the million-dollar question: knowing all this, what is the average middle-aged woman to do when told she doesn’t have to go through the whole humiliating
I think my main complaint is the declining sex drive … . Part of the problem is the fact that I feel like the Sahara desert down there. I want to have sex, but my body is not responding like it used to.
—Gail A. (49)
process? That menopause is inherently unnatural and unnecessary, and that for the price of a prescription, she can do an easy end run around all the hot flashes, the night sweats, and libido loss, holding on to her youth and vitality until she finally keels over at ninety? “Women will be emancipated only when the shackles of hormone deprivation are loosened!” “Menopause is completely preventable. No woman need suffer menopause or any of its symptoms if she receives preventative treatment before the onset of menopause!” Hearing such heady assurances, what forty-six-year-old wouldn’t feel a flutter of hope stirring in her ever-drooping bosom?
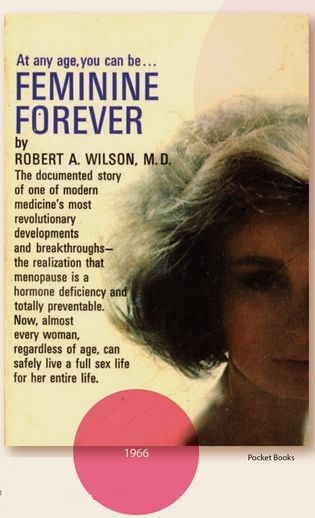
And that’s exactly how Dr. Robert A. Wilson, gynecologist and author of the bestselling 1966 book Feminine Forever, convinced so many women for years that long-term hormone replacement therapy (HRT) was the way to go. In the book’s intro, Dr. Robert B. Greenblatt eloquently lauded the seemingly selfless author: “Like a gallant knight he has come to rescue his fair lady not at the time of her bloom and flowering but in her despairing years; at a time of life when the preservation and prolongation of her femaleness are so paramount.”
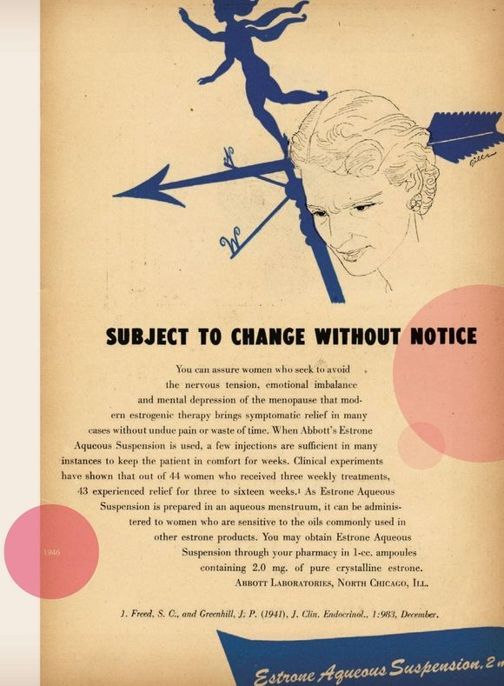
In fact, scientists had been searching for hormones, or at least for the way the brain communicated chemically to the body, since the 1800s. And when synthetic hormones were first created in the 1930s, they were quickly marketed for a variety of female ailments and conditions, in utter disregard for any potential health hazards.
Freud himself may have inadvertently started the HRT ball rolling by suggesting all women should be sedated when their periods ended, but tranquilizers and anti-depressants were a mere bowl of Beer Nuts once hormone therapy rolled along. The medicalization of menopause provided drug companies with an opportunity that was practically as good as printing money. By convincing women that all they needed was synthetic estrogen to make up for failing ovaries, thus sidestepping the inevitable pitfalls of aging, pharmaceutical companies struck a veritable gold mine—preying on widespread fear and ignorance.
In the mid-twentieth century, drug manufacturers didn’t have to prove a drug’s effectiveness; they only had to show it wasn’t inherently dangerous to the user. Nice that the FDA set the bar so high, wasn’t it? By the mid-1960s, after Wyeth effectively sold gynecologists on the powers of Premarin as a rejuvenator and mood stabilizer, 12 percent of postmenopausal women were regularly taking estrogen supplements. And yet it wasn’t until the publication of Forever Feminine in 1966 that HRTwent solid gold.
In his book, Wilson makes an untold number of totally unsubstantiated statements (i.e., lies and threats), apparently the crazier the better, in order to convince women of the powers of HRT: “Instead of being condemned to witness the death of their own womanhood … they will remain fully feminine.”“Women have the right to remain women. They shouldn’t have to live as sexual neuters for half their lives.” And why stop there? “Menopause is curable … . The bodily changes typical of middle age can be reversed and sexual function restored, along with a fully feminine appearance.” Our personal favorite: “Many physicians simply refuse to recognize menopause for what it is—a serious, painful, and often crippling disease.” Wilson goes on and on and on, including several weird, personal asides in which he shares his profound aversion for that current fashion trend, stretch pants.
We would like to be charitable and imagine Wilson to have been just the kind of guy his jacket blurb suggested: a chivalrous, Sean Connery-esque King Arthur out to rescue his beloved but aging Queen Guinevere from the horrors of decrepitude. But in fact, Wilson wasn’t a disinterested nonparticipant in the HRT campaign. Although it was barely mentioned at the time and is nowhere to be found in the book, both his research and Forever Feminine were quietly funded by Wyeth, producers of Premarin.
Eventually, the FDA banned Wilson from certain research; yet thanks to him, enthusiastic support for HRT continued for years. Magazines like Time sang its praises; Dr. David Reuben concurred with Wilson’s theories about menopausal women in his bestselling 1969 book, Everything You Always Wanted to Know About Sex (But Were Afraid to Ask): “As the estrogen is shut off, a woman comes as close as she can to being a man … . To many women, the menopause marks the end of their useful life.” As a result, estrogen sales went through the roof.
Pocket Books
But the mares’ urine hit the fan in 1975, when estrogen replacement therapy was linked with endometrial cancer. The New England Journal of Medicine, hardly a hotbed of medical hysteria, published disturbing reports showing that postmenopausal women taking estrogen supplements had fourteen times as much risk of developing endometrial cancer as women who didn’t. Estrogen sales came to a screeching halt, and by 1979, it was only prescribed for treating hot flashes and vaginal dryness. As a medical supertrend, estrogen therapy appeared to be going the way of the Hula Hoop and the Pet Rock.
But because all good horror stories demand a third act, there was a plot twist yet to come. Doctors discovered that the hormone progestogen would counteract the cancer-inducing properties of estrogen. What a relief! It was hormone therapy with all the cancer-causing kinks taken out. To launch its retooled product in the 1980s, Wyeth put together a hugely expensive marketing campaign, and as a result, Prempro, its new estrogen/progestogen combo pill, became a bona fide hit.
For a while, the combination of estrogen and progestogen seemed to be just the ticket: not only did it alleviate menopause symptoms, but it also protected bones from osteoporosis. What’s more, it was starting to look as if the hormone combo also prevented cardiac disease … happy news indeed for the Wyeth gang! By the 1990s, HRT for the postmenopausal woman was again a no-brainer, having successfully pulled itself back from the brink of medical obsolescence by again promising her she needn’t fear becoming either “a dull-minded but sharp-tongued caricature of her former self” or “one of the saddest of human spectacles” (more quotes from Wilson’s Feminine Forever).
And then, researchers finally got around to those long-term studies, to document HRT’s effectiveness. It turned out that women who already had heart disease were more likely to have a heart attack if on estrogen therapy. And in 2002, the bomb dropped. Women’s Health Initiative concluded that while HRT did have some health benefits—allaying osteoporosis and reducing the risk of colorectal cancer—these in no way outweighed the increased risk for blood clots, heart disease, stroke, and breast cancer.
Talk about a buzz kill. The National Institutes of Health abruptly ended the study, sending its sixteen thousand participants letters recommending they stop taking the drugs. The NIH sent out a press release in December, adding “steroidal estrogens” to its known carcinogen list, calling out estrogen in both replacement therapy and birth control pills as a potential cancer-causing agent.
And yet the HRT story still isn’t over. Reluctant to relinquish such a dependable source of vast revenue, Wyeth introduced even lower-dose versions of Prempro for treating osteoporosis and postmenopausal symptoms in 2003. But in October 2007, a jury awarded a $134.5 million verdict to three Nevada women who argued that Premarin and Prempro were responsible for their breast cancer. There are currently over five thousand similar lawsuits in state and federal courts across the country.
In spite of the bad press and the stream of lawsuits, drug companies are still actively marketing their hormonal wares. These days, however, manufacturers market hormone therapy more realistically for short-term symptom relief than as a long-term elixir of dewy youth. And yet it’s clear women are still being misled by assurances like the following from
premarinonline.com
: “PREMARIN can help guide you through this graceful transition. Because PREMARIN has been women’s best friend for over 60 years and will always be.”With friends like that, who needs asbestos?
Yet all is not lost for perimenopausal women. In her 2006 book, The Wisdom of Menopause, Dr. Christiane Northrup suggests that instead of limiting themselves to just prescription drugs from big pharma, perimenopausal women should also consider supplementing their dwindling hormone levels in alternative ways, such as with herbs and diet. She sings the praises of foods like soy and flaxseed, which are rich in the natural hormones found in plants, as well as certain berries and grains, which contain bioflavonoids.
More intriguing, Northrup also suggests that we ditch the whole one-size-fits-all way of thinking about hormone replacement. She advises working with one’s physician and special pharmacists to develop an individualized hormone replacement plan made up of“bioidentical hormones,” customized to one’s own needs and symptoms.
Bioidentical hormones can’t be patented, which means you won’t be finding them manufactured by the big pharmaceuticals anytime soon. And long-term studies have yet to be conducted, so their safety over time remains an open question. That being said, they don’t seem to have the same carcinogenic effect as Premarin or Premproat least not at individualized, low doses for short-term relief. Northrup suggests that bioidentical hormones, as well as dietary supplementation, are two viable options for women who are understandably leery of not only the symptoms of menopause, but of the conventional “cure” itself.