i bc27f85be50b71b1 (7 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown


10 AClJTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
duction can decrease CO (refer to the discussion of rhythm and conduction disturbances in the Pathophysiology section)?
Netlral lnptlt
The SA node has its own inherent rate. Neural input can, however,
influence HR, HRV, and contractility through the autonomic nervous
system.J•s
Parasympathetic system (vagal) neural input generally decelerates
cardiac function, thus decreasing HR and contractility. Parasympathetic input travels through the vagus nerves. The right vagus nerve primarily stimulates the SA node and affects rate, whereas the left vagus nerve primarily stimulates the AV node and affects AV conduction.J,8
Sympathetic system neural input is through the thoracolumbar
sympathetic system and serves to increase HR and augment ventricular contractility, thus accelerating cardiac function.3
Endocrine Input
In response to physical activity or stress, a release in catecholamines
increases HR, contractility, and peripheral vascular resistance for a
net effect of increased cardiac function.' Refer to Table 1-3 for the
cardiac effects of hormones.
Local Input
Tissue pH, concentration of carbon dioxide (C02), concentration of oxygen (02)' and metabolic products (e.g., lactic acid) can affect vascular tone.' During exercise, increased levels of CO2, decreased levels of 02'
decreased pH, and increased levels of lacric acid ar the tissue level dilate
local blood vessels and therefore increase CO distribution to thar area.
Cardiac Reflexes
Cardiac reflexes influence HR and contractility and can be divided
into three general categories: baroreflex (or pressure), Bainbridge
reflex (or stretch), and chemoreflex (or chemical reflexes).


CARDIAC SYSTEM
1 t
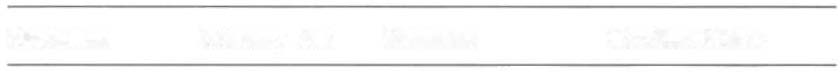
Table 1-3. Cardiac Effects of Hormones
Hormone
Primary Site
Stimulus
Cardiac Effect
Norepinephrine Adrenal
Stress/exercise
Vasoconstriction
medulla
Epinephrine
Adrenal
Stress/exercise
Coronary artery
medulla
vasodilation
Angiotensin
Kidney
Decreased arte-
Vasoconstriction,
rial pressure
increases blood
volume
Vasopressin
Posterior
Decreased arte-
Potem vasoconstriaor
pituitary
rial pressure
Bradykinin
Formed by
Tissue damage!
Vasodilation,
polypep-
inflammation
increased capil-
tides in
lary permeabiliry
blood when
activated
Histamine
Throughout
Tissue damage
Vasodilation,
tissues of
increased capil-
body
lary permeability
Atrial natri-
Atria of heart
Increased atrial
Decreased blood
uretic pep-
stretch
volume
tides
Aldosterone
Adrenal
Angiotensin II
Increases blood
cortex
(stimulated) by
volume, kidneys
hypovolemia
excrete more
or decreased
potassium
renal perfusion
Source: Data from AC Guyton.JE Hall. Textbook of Medical Physiology (9th cd). Phil-
adelphia: Saunders, 1996.
Baroreflexes are activated through a group of mechanoreceptors
located in the heart, great vessels, and intrathoracic and cervical
blood vessels. These mechanoreceptors are most plentiful in the walls
of the internal carotid arteries.] Mechanoreceptors are sensory receptors that are sensitive co mechanical changes, such as pressure and Stretch. Activation of the mechanoreceptors by high pressures results
in an inhibition of the vasomotor center of the medulla that increases
vagal stimulation. This chain of events is known as the baroref/ex and
results in vasodilation, decreased HR, and decreased contractility.

12
ACUTE CARE HANDBOOK ';OR PHYSICAL THERAPISTS
Mechanoreceptors located in the right atrial myocardium
respond to stretch. With an increased volume in the right atrium,
there is an increase in pressure on the atrial wall. This reflex,
known as the Bail1bridge reflex, stimulates the vasomOtor center of
the medulla, which in turn increases sympathetic input and
increases HR and contractility.) Respiratory sinus arrhythmia, an
increased HR during inspiration and decreased HR during expiration, may be facilitated by changes in venous return and SV caused by changes in thoracic pressure induced by the respiratory cycle.
At the beginning of inspiration, when thoracic pressure is
decreased, venous return is greater, and therefore there is a greater
stretch on the atrial wall .'
Chemoreceptors located on the carotid and aortic bodies have a
primary effect on increasing rate and depth of ventilation in response
to CO, levels, but they also have a cardiac effect. Changes in CO,
during the respiratory cycle may also result in sinus arrhythmia.3
Coroltary Perfusiolt
For a review of the major coronary arteries, refer to F igure I - I . Blood
is pumped to the large superficial coronary arteries during ventricular
systole. At this time, myocardial contraction limits the flow of blood
to the myocardium; therefore, myocardial tissue is actually perfused
during diastole.
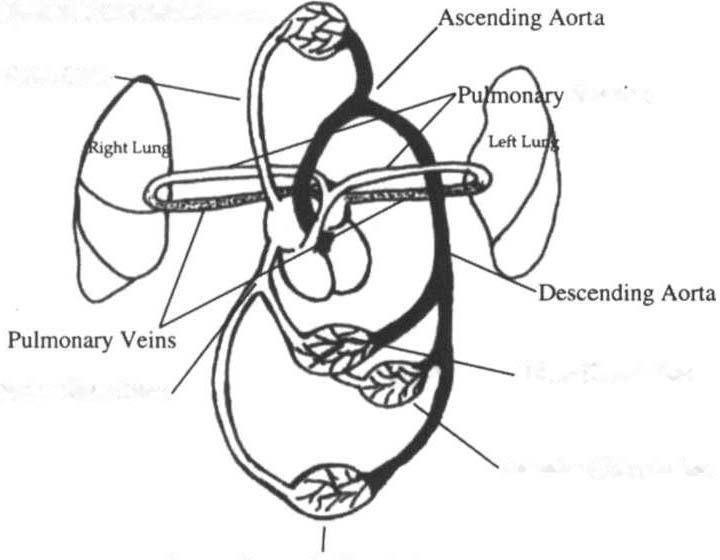
Systemic Circulatiolt
For review of the primary anatomic structures and distribution of
the systemic circulation, refer to F igure ] -4. Systemic circulation is
affected by roral peripheral resistance (TPR), which is the resistance to blood flow by the force created by the aorta and arterial system. Two factors that contribute to resistance are ( 1 ) vasomotor
tone, in which vessels dilate and constrict, and (2) blood viscosity,
in which greater pressure is required to propel thicker blood. Also
called systemic vasClilar resistaltce, TPR and CO influence blood
pressure (BP).3 This relationship is illustrated in the following
equation:
BP = CO xTPR