i bc27f85be50b71b1 (11 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

22 AClJfE CARE HANDBOOK FOR PHYSICAL THERAPISTS
0--
Supine
Sitting
Standing
Figure 1-7. Orthostatic blood pressure symbols.
• The same extremity should be used when serial BP
recordings will be compared for an evaluation of hemodynamic response.
• A BP record is kept on the patient's vital sign flow sheet.
This is a good place to check for BP trends throughout the
day and, depending on your hospital's policy, to document
BP changes during the therapy session.
•
An auscultatory gap is the disappearance of sounds
between phase 1 and phase 2 and is common in patients
with high BP, venous distention, and severe aortic stenosis.
Its presence can create falsely low systolic pressures if the
cuff is not inflated high enough (which can be prevented
by palpating for the disappearance of the pulse prior to
measurement), or falsely high diastolic pressures if the
therapist stOps measurement during the gap (prevented by
listening for the phase 3 to phase 5 transitions). 13
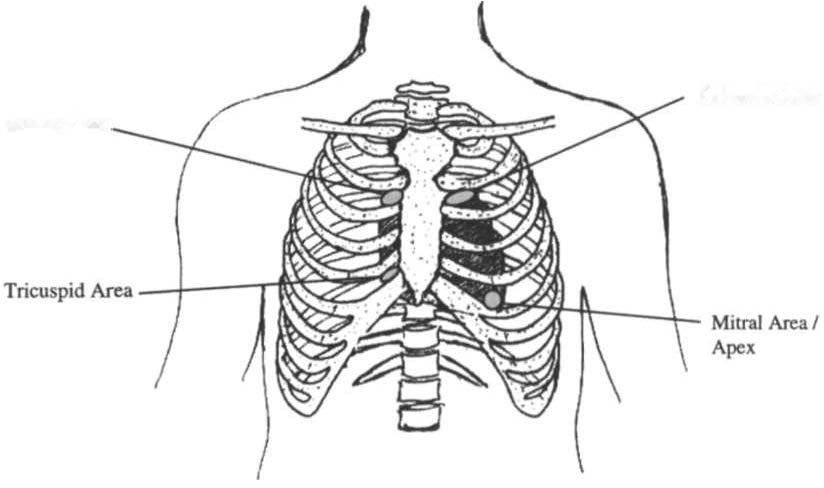
Auscultation
Evaluation of heart sounds can yield information about the patient'S
condition and tolerance to medical treatment and physical therapy
through the evaluation of valvular function, rate, rhythm, valvular
compliance, and ventricular compliance.4 To listen to heart sounds,
a stethoscope with both a bell and a diaphragm is necessary. For a
review of normal and abnormal heart sounds, refer to Table 1-9.
The examination should follow a systematic pattern using both the
bell (for low-pitched sounds) and diaphragm (for high-pitched
sounds) and should cover all auscultatory areas, as illustrated in


CARDIAC SYSTEM
23
Table 1-9. Normal and Abnormal Heart Sounds
Sound
Location
Description
5 1 (normal)
All areas
First heart sound, signifies closure of
atrioventricular valves and corresponds to onset of ventricular systole.
52 (normal)
All areas
Second heart sound, signifies closure of
semilunar valves and corresponds
with onset of ventricular diastole.
53 (abnormal) Best appreciated
Immediately following S2, occurs early
at apex
in diastole and represents filling of
the ventricle. In young healthy individuals, it is considered normal and
called a physiologic third sound. In
the presence of heart disease, it
results from decreased ventricular
compliance (a classic sign of congestive heart failure).
54 (abnormal) Best appreciated
Immediately preceding S l , occurs late
at apex
in ventricular diastole, associated
with increased resistance to ventricular filling; common in patients with
hypertensive heart disease, coronary
heart disease, pulmonary disease, or
myocardial infarction, or following
coronary artery bypass grafts.
Murmur
Over respective
Indicates regurgitation of blood
(abnormal)
valves
through valves; can also be classified
as sysrolic or diastolic ll1llfmurs.
Common pathologies resulting in
murmurs include mitral regurgitation and aortic stenosis.
Pericardia I
TIlird or fourth
Sign of pericardial innammation (perifriction rub
inrercostal
carditis), associated with each beat of
(abnormal)
space, anrerior
the hearr, sounds like a creak or
axillary line
leather being rubbed together.
Source: Data from LS Bickley. Bate's Guide to Physical Examination and Hisfory
Taking 17th cd). Philadelphia: Lippincott, 1999.
24 AClITE CARE HAND nOOK FOR I)I·IYSICAL THERAPISTS
Pulmonic Area
Aortic Area
Figure 1-8. Areas for heart sound auscultation. (Drawn by Barbara Cocanour.
Ph.D., University of Massac/msetts, Loweff. Departmel1l of Physical Therapy.)
Figure 1-8. Abnormal sounds should be noted with a description of
the conditions in which they were heard (e.g., after exercise or during exercise).
Clinical Tip
• Always ensure proper function of stethoscope by tapping
the diaphragm before applying the stethoscope to the patient.
• Rubbing the stethoscope on extraneous objects can add
noise and detract from true examination.
• Auscultation of heart sounds over clothing should be
avoided, because it muffles the intensity of both normal
and abnormal sounds.
• If the patient has an irregular cardiac rhythm, HR
should be determined through auscultation (apical HR).
To save time, this can be done during a routine auscultatOry examination with the stethoscope's bell or diaphragm
in any location.


CARDIAC SYSTEM
25
Diagnostic and Laboratory Measures
The diagnostic and laboratory measures discussed in this section provide information that is used to determine medical diagnosis, guide interventions, and assist with determining prognosis. The clinical relevance of each test in serving this purpose varies according to the pathology. This section is organized across a spectrum of least invasive to most invasive measures. When appropriate, the test results mOst pertinent to the physical therapist are highlighted. Information
that bears a direct impact on physical therapy clinical decision making usually includes that which helps the therapist identify indications for intervention, relative or absolute contraindications for intervention, possible complications during activity progression, and indicators of performance.
Oximetry
Oximetry (Sa02) is used to indirectly evaluate the oxygenation of a
patient and can be used to titrate supplemental oxygen. Refer to
Chapter 2 for a further description of oximetry.
Electrocardiogram
ECC provides a graphic analysis of the heart's electrical activity.
The ECC is commonly used to detect arrhythmias, heart blocks,
and myocardial perfusion. It can also detect atrial or ventricular
enlargement. ECC used for continuous monitoring of patients in
the hospital typically involves a two- or three-lead system. A lead
represents a particular portion or "view" of the heart. The
patient'S rhythm is usually displayed in his or her room, in the hall,
and at the nurses' station. Diagnostic ECC involves a 1 2-lead analysis, the description of which is beyond the scope of this book. For a review of basic ECC rate and rhythm analysis, refer to Table 1-10
and Figure 1-3.
Holter Monitoring
Holter monitoring is 24- or 48-hour ECC analysis. This is performed to detect cardiac arrhythmias and corresponding symptoms during a patient'S daily activity.12 Holter monitoring is different than telemetric monitoring because the ECC signal is
