i bc27f85be50b71b1 (8 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown


CARDIAC SYSTEM
13
Upper Systemic Circulation __
Superior Vena Cava
Anenes
Liver Circulation
Inferior Vena Cava
Intestinal Circulation
Lower Systemic Circulation
Figure 1-4. Schematic of systemic circulation. (Draw'J by Barbara Cocanoll"
Ph.D., University of Massachusetts, Lowel1, Department of Physical Therapy.)
Cardiac Evaluation
Cardiac evaluarion consists of patient history, physical examination (which consists of observation, palpation, BP measurement, and heart sound auscultation), laboratory rests, and diagnostic
procedures.
Patiellt History
In addition to the general charr review presented in Appendix I-A,
pertinent information about patients with cardiac dysfunction that
should be obtained before physical examination includes the
following'· 10-12:
• Presence of chest pain (see Appendix X for an expanded
description of characteristics and etiology of chest pain)



14 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
1. Location, radiation
2. Character and quality (crushing, burning, numbing, hot)
and frequency
3. Angina equivalents (what the patient feels as angina, e.g.,
jaw pain, shortness of breath, dizziness, lightheadedness, diaphoresis, burping, nausea, or any combination of these)
4. Aggravating and alleviating factors
5. Precipitating factors
• Medical treatment sought and its outcome
• Presence of palpitations
• Presence of cardiac risk factors (Table 1-4)
• Family history of cardiac disease
Table 1-4. Cardiac Risk Faccors
Major
Independent
Risk FactOrs
Predisposing Risk Factors
Conditional Risk Factors
Smoking
Physical inactivity
Elevated triglycerides
Hypertension
Obesity
Small LDL parricles
Elevated serum
Body mass index
Elevated homocysteine
cholesterol,
>30 kglm'
Elevated lipoprotein (a)
roral (and LDLI
Abdominal obesity (waisthip ratio)
Decreased high
Men >40 in.
Elevated inflammatory
density lipopromarkers
tein cholesterol
Diabetes mellitus
Women >35 in.
C-reactive protein
Advancing age
Family history of prema
Fibrinogen
ture heart disease
Psychosocial factors
Ethnic characteristics
LDL = low-density lipoprotein.
Source: Data from SM Grundy, R Pasternak, P Greenland, et al. Assessment of cardiovascular risk by use of multiple-risk-factOr assessmenr equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology, Circulation 1999; 100: 1481-1492.

CARDIAC SYSTEM
15
o History of dizziness or syncope
o Previous myocardial infarction (MI), cardiac studies, or procedures
Clinical Tip
• When discussing angina with a patient, use the patient'S
terminology. If the patient describes the angina as "crushing" pain, ask the patient if he or she experiences the crushing feeling during treatment as opposed to asking the
patient if he or she has chest pain.
o The common medical record abbreviation for chest
pain is CPo
Physical Exam;1Iatio1l
Observation
Key components of the observation portion of the physical examination include the following··7:
1 .
Facial color, skin color and rone, or the presence of diaphoresis
2.
Obvious signs of edema in the extremities
3.
Respiratoty rate
4.
Signs of trauma (e.g., paddle burns or ecchymosis from cardiopulmonary resuscitation)
5.
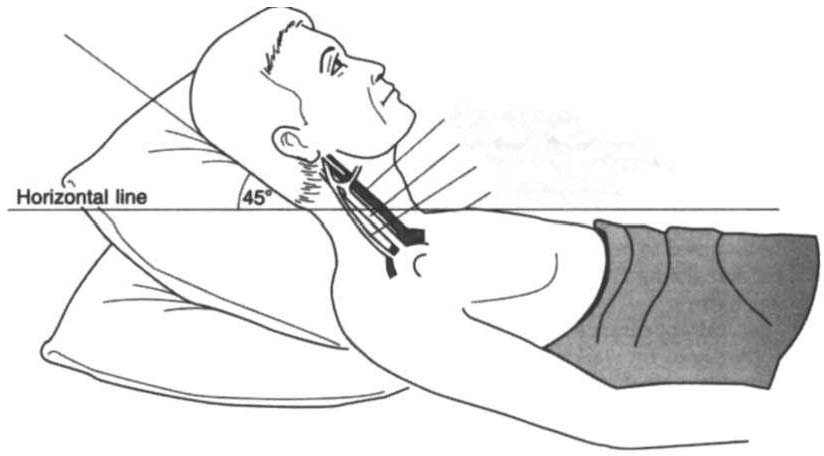
Presence of jugular venous distention, which results from
the backup of Auid into the venous system from right-sided CHF
(Figure 1-5)
a. Make sure the patient is in a semirecumbent position (45
degrees).
b. Have the patient turn his or her head away from the side
being evaluated.
c. Observe pulsations in the internal jugular neck region.
Pulsations are normally seen 3-5 em above the sternum. Pul-

1 6 ACUTE CARE HANDBOOK FOR PHYSICAL TI-IERAPISTS
CaroHd artery
In1ernal jugular veJn
External Jugular vein
Sternal angle
Figure 1-5. Measurement of iugular venous distention (J VPJ. The J VP reading is the maximum height, in centimeters, above the sternal angle at which venous pulsations are visible.
sations higher than this or absent pulsations indicate jugular
venous distention.
Palpation
Palpation is the second component of the physical examination and is
used to evaluate and identify the following:
•
Pulses for circulation qua�ty, HR, and rhythm (Table 1-5, Figure 1-6)
•
Exttemities for pitting edema bilaterally (Table 1-6)
