i bc27f85be50b71b1 (5 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

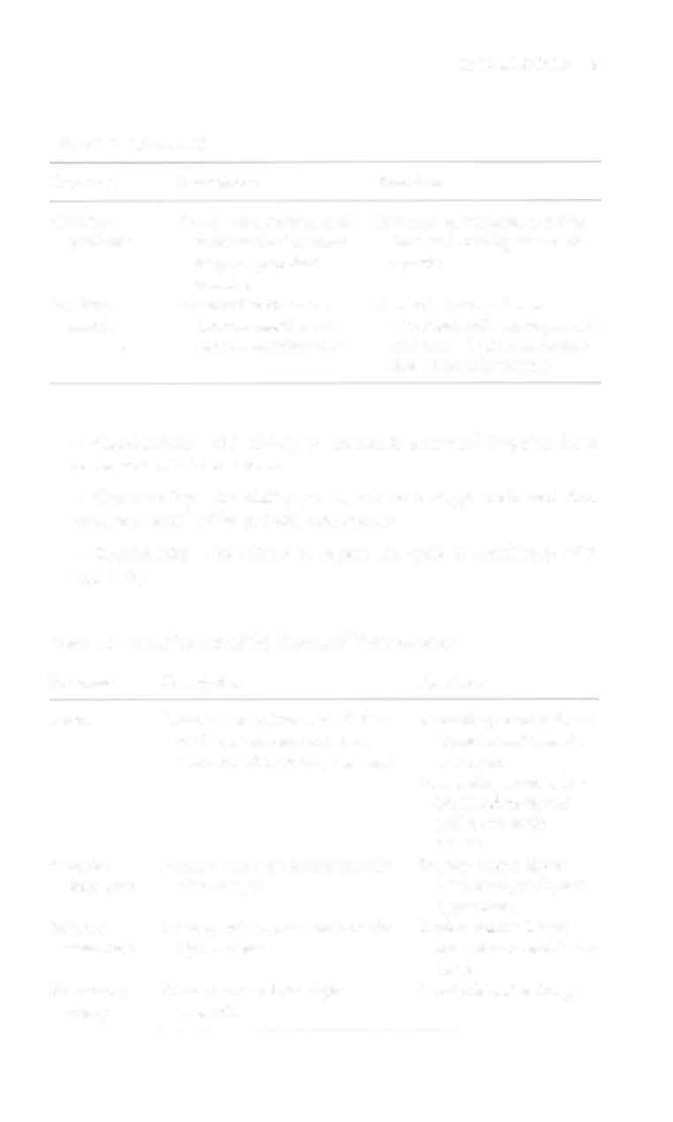
diac wall, covers surtrauma
face of heart and great
vessels
Myocardium
Central layer of thick
Provides major pumping force
muscular tissue
of the venrricles
Endocardium
Thin layer of endothe
Lines [he inner surface of hearr,
liurn and connective
valves, chordae rendineae,
tissue
and papillary muscles
Right atrium
Heart chamber
Receives blood from venous
system and is a primer
pump for the right ventricle
Tricuspid
Atrioventricular valve
Prevents back flow of blood
valve
between right atrium
from right ventricle to
and ventricle
atrium during ventricular
systole
Right
Hearr chamber
Pumps blood to pulmonary
ventricle
circulation
Pulmonic
Semilunar valve between
Prevents back flow of blood
valve
right ventricle and
from pulmonary artery to
pulmonary arrery
right ventricle during diastole
Left atrium
Heart chamber
Acts as a reservoir for blood
and primer pump for left
ventricle
Mitral valve
Atrioventricular valve
Prevents backflow of blood
between left atrium
from left ventricle to
and ventricle
atrium during ventricular
systole
Left ventricle
Heart chamber
Pumps blood to systemic circulation
Aortic valve
Semilunar valve between
Prevents backflow of blood
left ventricle and aorta
from aorta to left ventricle
during ventricular diastole


CARDIAC SYSTEM
5
Table 1-1. Continued
Structure
Description
Function
Chordae
Tendinous attachment of
Prevents valves from everting
tendineae
atrioventricular valve
into atria during ventricular
cusps to papillary
systole
muscles
Papillary
Muscle that connects
Constricts and pulls on
muscle
chordae tendineae to
chordae tendineae to prevent
floor of ventricle wall
eversion of valve cusps during ventricular systole
• Conductivity-the ability to transmit electrical impulse from
cell to cell within the heart
• Contractility-the ability to stretch as a single unit and then
passively recoil while actively contracting
• Rhythmicity-the abiliry to repeat the cycle in synchrony with
regularity
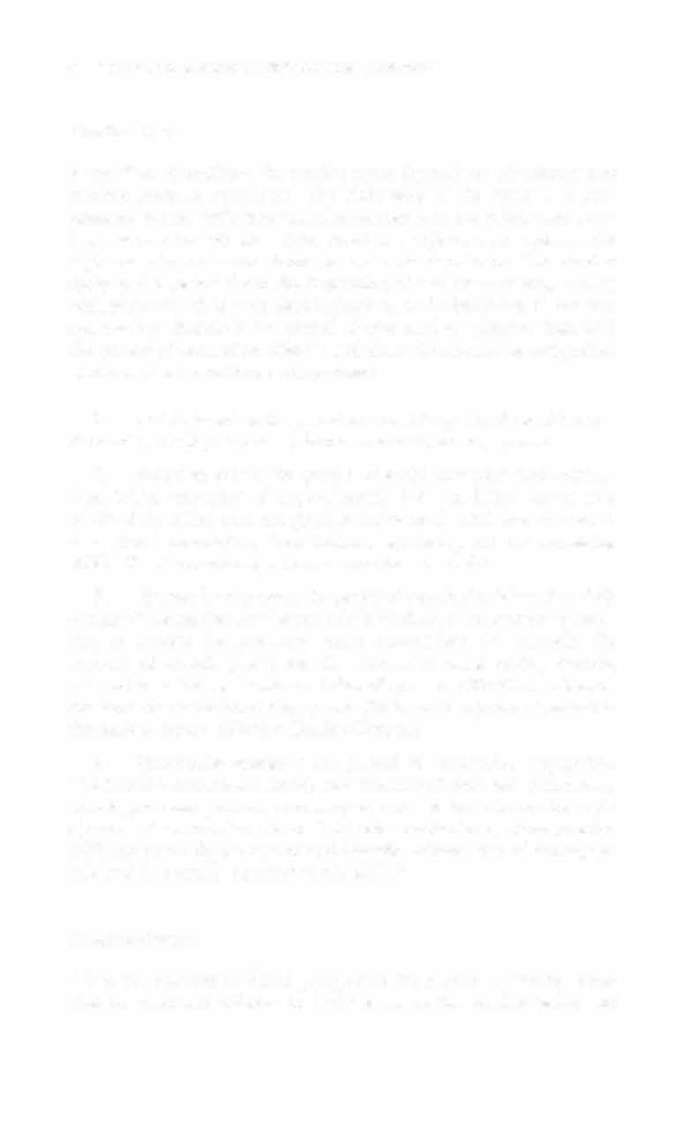
Table 1-2. Great Vessels of the Heart and Their Function
Structure
Description
Function
Aorta
Primary artery from the left ven-
Ascending aorta delivers
tricle that ascends and then
blood to neck, head,
descends after exiting the heart
and arms.
Descending aorta deliv-
ers blood to visceral
and lower body
tissues.
Superior
Primary vein that drains into the
Drains venous blood
vena cava
right atrium
from head, neck, and
upper body.
Inferior
Primary vein that drains into the
Drains venous blood
vena cava
right atrium
from viscera and lower
body.
Pulmonary
Primary artery from right
Carries blood to lungs.
artery
ventricle
6
AarrE CARE HANDBOOK FOR PHYSICAL THERAPISTS
Cardiac Cycle
Blood flow throughout the cardiac cycle depends on circulatOry and
cardiac pressure gradients. The right side of the heart is a lowpressure system with little vascular resistance in the pulmonary arteries, whereas the left side of the heart is a high-pressure system with high vascular resistance from the systemic circulation. The cardiac
cycle is the period from the beginning of one contraction, starting
with sinoatrial (SA) node depolarization, to the beginning of the next
contraction. Systole is the period of contraction, whereas diastole is
the period of relaxation. SystOle and diastOle can also be categorized
into atrial and ventricular components:
1 . Atrial diastole is the period of atrial filling. The flow of blood is
directed by the higher pressure in the venous circulatory system.
2.
Atrial systole is the period of atrial emptying and cOntrac-
tion. Initial emptying of approximately 70% of blood occurs as a
result of the initial pressure gradient between the atria and the ventricles. Atrial contraction then follows, squeezing our the remaining 30%.3 This is commonly referred to as the atrial kick.
3.
Ventricular diastole is the period of ventricular filling. It initially
occurs with ease; then, as the ventricle is filled, atrial contraction is necessary to squeeze the remaining blood volume into the ventricle. The amount of stretch placed on the ventricular walls during diastOle,
referred to as left ventricular end diastolic pressure (LVEDP), influences
the force of contraction during systOle. (Refer to description of preload in
the section Factors Affecting Cardiac Output.)
4.
Ventricular systole is the period of ventricular contraction.
The initial contraction is isovolumic (meaning it does nOt eject blood),
which generates pressure necessary to serve as the catalyst for rapid
ejection of ventricular blood. The left ventricular eiectiOlt fraction
(EF) represents the percent of end diastOlic volume ejected during systOle and is normally approximately 60%.3
Cardiac Output
CO is the quantiry of blood pumped by the heart in 1 minute. It can
also be described relative to body mass as the cardiac index, the


CARDIAC SYSTEM
7
amount of blood pumped per minute per square meter of body mass.
Regional demands for tissue perfusion (based on local metabolic needs)
compere for systemic circularion, and roral CO adjusts ro meet these
demands. Adjustment ro CO occurs with changes in hearr rate (HR)
(chronotropic) or stroke volume (SV) (inotropic).· Normal resting CO
is approximarely 4-8 liters per minute, and normal cardiac index is
approximately 2.5-4.0 liters per minute per meter'·' (with a resting HR
of 70 beats per minute [bpml, resring SV is approximately 71 ml/beat).
The maximum value of CO represents the functional capacity of the
circulatory system to meet the demands of physical activity.
CO (liters per minute) = HR (bpm) x SV (liters)
Facrors Affecting Cardiac Output
