Meatonomics (18 page)
Authors: David Robinson Simon

The predictable elements of cholesterol and saturated fats aren't the only things in meat that will do you harm. In fast-paced industrial slaughter operations, where workers process as many as three hundred animals an hour, a little feces invariably winds up in much of the end product. Such processing methods have given rise to a persistent epidemic of food-borne disease. This year, fecal pathogens will sicken one in four Americans and hospitalize three hundred thousand.
48
Two of the most common pathogens, campylobacter and salmonella, together will cause almost half of these incidents.
49
These organisms
routinely live in the intestines of normal, healthy farm animals like pigs, chickens, and cattle, and are transmitted to humans via fecal matter. If you've ever had nausea, diarrhea, or a gurgling belly right after a meal, there's a good chance you ate something contaminated with live fecal bacteria. The problem has been eloquently summarized by Eric Schlosser, author of
Fast Food Nation
: “There's shit in the meat.”
50
In fact, the shit is hitting the fan. Fecal contamination is widespread, affecting all kinds of meat in virtually all US grocery stores, and the situation continues to get worse. A 2007 Consumer Reports study found campylobacter and salmonella bacteria in four out of five packaged chickens for sale in supermarkets and other retailers across the United States.
51
This discovery represented a big increase from the group's 2003 study, which found these bacteria in only half of chickens tested. Inexplicably, the expensive, organic chickens were more likely to contain salmonella than the inexpensive, inorganic chickens.
52
Ground meat often contains fecal bacteria. One reason is that producers typically process multiple carcasses through a single grinder, giving bacterial contamination in the equipment an opportunity to spread from batch to batch. A USDA analysis of hamburger meat from hundreds of US slaughterhouses found fecal bacteria in four out of five samples.
53
In another study, federal agencies found
E. coli
in eight of ten ground turkey samples and seven of ten ground beef samples sold at hundreds of retail outlets throughout the United States.
54
Yet while ground meat is routinely contaminated, whole meat isn't much better. Thus, the feds also found
E. coli
in nearly nine out of ten chicken breasts and four out of ten pork chops sold.
55
Unfortunately, organically raised animals are usually butchered in factories at the same frantic pace as ordinary animals, so paying extra for the organic label doesn't make fecal contaminants any less pervasive.
By the way, don't be confused by the fact that fecal bacteria sometimes wind up on vegetables. In 2006, for example, more than two hundred people were sickened and three died from eating spinach contaminated with
E. coli
. But plants don't create feces; fecal bacteria
begin their lives in the guts of animals. Thus, the 2006 spinach incident was traced back to cattle and pigs.
56
In factory farms across the United States, antibiotics are routinely fed to cattle, pigs, and poultry to promote growth and control disease.
57
In fact, in today's animal agriculture industry, where organic producers are as rare as hens' teeth, dosing animals with drugs is almost as common as feeding them. Unless and until the FDA takes steps to ban their use, these drugs will continue to figure prominently in Americans' meat, eggs, and dairy.
American farm animals consume 28 million pounds of antibiotics yearly, much of it to promote growth (rather than help the sick, as the drugs were intended). By comparison, Americans take about 7 million pounds of antibiotics per year, and then only to combat infection. For the consumer down the line, the practice of dosing farm animals leaves antibiotic residues in the meat, and it weakens the therapeutic effect of those antibiotics if needed someday to combat infection. Perhaps even worse, this practice of killing the weakest bacteria but letting the hardiest survive has given rise to drug-resistant bacteria that are difficult to combat in both animals and humans.
If the presence of residual drugs in your food makes you uncomfortable, the advocates at the Animal Health Institute (AHI), a trade group for animal-drug makers, are at the ready to reassure you. “Many published studies,” states AHI in a promotional brochure, “have found that the risk to humans from resistant bacteria derived from eating meat or poultry from animals treated with antibiotics is
extremely minimal.
”
58
Does this sound at all like the 1950s-era Chesterfield cigarette ads that informed readers of a “study” that found smoking Chesterfields did not “adversely affect” the “ears, nose, throat and accessory organs” of smokers?
59
In fact, a steady stream of published research starting in the 1970s shows that antibiotic use in animals causes a number of far-from-minimal health problems for humans, including allergic reactions, promotion of drug-resistant bacteria, and inefficacy of antibiotics when used therapeutically.
60
The tendency for humans and farm animals to develop increased resistance to antimicrobial drugs is serious enough that in 1996, four federal agencies formed the National Antimicrobial Resistance Monitoring System (also known by the catchy acronym NARMS). Every year, NARMS analyzes drug-resistant pathogens in US retail meat and publishes its findings. Its latest report isn't pretty. There's been a proliferation over the past decade of various antimicrobial-resistant bacteria, including salmonella strains that develop in pigs, cattle, and chickens. These microorganisms have also grown steadily hardier and more drug-resistant since 1996.
61
If that's not enough to worry about, the report found an increase in unusually highly resistant
E. coli
strains in chicken breasts, ground beef, and pork chops as well.
62
Beyond fostering new and more virulent strains of bacteria, the rampant combination of antibiotics and farm animals has promoted the innocuous-sounding but evil MRSA.
63
MRSA, or methicillin-resistant
Staphylococcus aureus
, is a staph infection that can lead to pneumonia, blood poisoning, toxic shock syndrome, heart-valve infection, and death. MRSA is particularly scary because of its resistance to methicillin, amoxicillin, penicillin, oxacillin, and other antibiotics. This highly adaptive organism responds to each new antibiotic it encounters by evolving genetically until the antibiotic is useless against it. Charles Darwin would be fascinated—this is natural selection, pure and simple. Single-cell bacteria evolve a lot faster than humans, and in case of MRSA, animal antibiotics are helping this organism win the race. Moreover, although we commonly associate the spread of MRSA with hospital wards, some of the disease's strains are known to have started among farm animals and spread to humans through contact with farm workers.
64
A 2011 study found MRSA in nearly half of all meat samples collected from retail stores around the United States. Three-quarters of turkey samples contained the malevolent bacteria, as did two out of five samples of pork, chicken, and beef.
65
While cooking generally kills the bacteria and is advisable if you eat any industrially produced meat, those handling uncooked meat can become infected just from contact.
The cocktail of farm animal drugs doesn't end there. Another chemical used to boost profits from industrial meat and dairy is growth hormone. As we saw in
chapter 4
, the FDA has approved the controversial growth hormone rBST for use in dairy cows. At the same time, most US beef cattle are implanted with a cocktail that may include sex hormones like androgens (testosterone substitutes), estrogens (primary female sex hormones), and progestins (agents that halt a female's estrus cycle). Some of these growth hormones are the same controversial and harmful anabolic steroids used by athletes to increase muscle mass. But forget looking like former home-run king Mark McGwire someday—when these dietary factors alter the human body's hormone balance even slightly, the effects can be damaging—particularly in fetuses and children.
One study found evidence of decreased fertility among children of mothers who ate large amounts of hormone-implanted beef during pregnancy.
66
Hormones in beef are also blamed for early puberty onset among children in Italy and Puerto Rico.
67
Because of such research, the European Union forbids all use of hormones in farm animals and even caused a mini–trade war with the United States by banning the sale or import of hormone-implanted beef. Yet the FDA, for its part, continues to permit hormone use in cattle, downplaying or ignoring the associated health risks.
We can blame meatonomics for the high levels of contaminants and residues in American animal foods. Humans managed to raise farm animals for millennia without giving them steroids and antibiotics, and as organic farming shows, we can readily do so when we choose. And when animals are slaughtered and processed carefully (although, as a result, at greater expense), feces are not routinely packaged with the meat. But meatonomics is a bulk business. It focuses on quantity over quality, on profitability over the health or comfort of humans and animals. Dosing animals with antibiotics and steroids helps the bottom line by increasing output, so it's developed into a bedrock meatonomics principle.
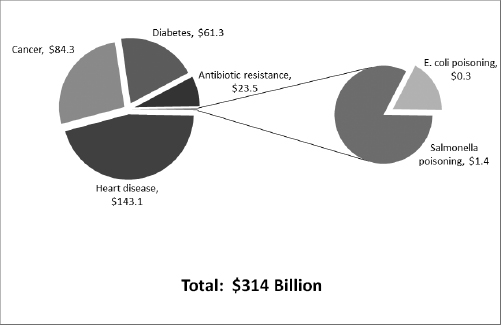
We've seen the diseases. Now let's look at the doctors' bills. Based on research that shows the annual human medical costs related to
E. coli
and salmonella cases are $3.4 billion yearly, the portion of those costs associated with these pathogens transmitted by animal foods is an estimated $1.7 billion.
68
In the antibiotics department, the total annual health care cost related to antibiotic resistance in humans is roughly $47.2 billion, and the portion related to farm animals is estimated at half of that—or $23.6 billion.
69
Adding this number to the fecal contamination figures yields a ballpark total of $25.3 billion in annual, externalized human health care costs related to contaminants and antibiotics in our animal foods. But these costs, although huge, are just a drop in the health care bucket.
The annual costs of treating cancer, diabetes, and heart disease are massive—and growing. In 1980, total US health care costs were $706 billion (in today's dollars).
70
Today, we're spending three-quarters of that figure just treating the big three. Add in the additional expenses related to lost productivity—which we must do to gauge the full losses stemming from these illnesses—and the total costs of just these three illnesses rocket to more than $900 billion. Heart disease tops the list with total annual US costs of $477 billion,
71
followed by cancer with a total of $253 billion.
72
Type 2 diabetes is a close third at $184 billion.
73
Of course, these diseases have a number of contributing causes, and diet is just one. Nevertheless, studies show that a diet high in unhealthy substances like cholesterol and saturated fats (that is, one based primarily on animal foods) is a significant factor in the development of these diseases. While definitive numbers showing the particular incidence of these diseases attributable to animal food consumption are not yet available, the medical literature does provide plenty of helpful guidance on the topic. Data support the estimates that a diet based on animal foods is responsible for roughly 30 percent of heart disease cases and roughly one-third of cancer and diabetes cases.
74
The cases of these three diseases caused by animal foods thus generate costs totaling roughly $289 billion yearly.
75
Adding to this
figure the $25 billion in costs related to contaminants and additives brings the total to $314 billion. As the largest component of the external costs of animal foods, the US health care expenses of consuming these items could bankrupt a country. In fact, it's cheaper for India and Finland to run both their governments for a year.
CHART 6.2
Externalized Health Care Costs of US Animal Agriculture (in billions of dollars)