Pediatric Examination and Board Review (127 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(D) depo-medroxyprogesterone
(E) progestin-only pills
19.
The patient has been on the pill for 2 weeks and now calls you to let you know she is bleeding again. After telling you emphatically that her compliance has been perfect, she explains that she has no cramping or fever and she is using about 2-3 pads a day. She has not been sexually active for the past 7 weeks and denies being on any other medication. What would you do at this time?
(A) admit her to the hospital for evaluation
(B) change the pill to one with a higher estrogen content
(C) prescribe an NSAID (ibuprofen or naproxen) to decrease the flow
(D) change her to progestin-only pills
(E) B or D
ANSWERS
1.
(E)
The menstrual history should always include the first day of the last menstrual period, duration and amount of bleeding, interval, and regularity of menses. In this case, it will also be important to ask about ongoing abdominal or pelvic pain, any history of abnormal bleeding from other sites (purpura, epistaxis, hematuria), weight changes, stress, recent use of hormonal and nonhormonal medication, and substance abuse. The date of her most recent vaginal intercourse should be helpful for adequate interpretation of the pregnancy test.
2.
(B)
The normal menstrual cycle is characterized by a follicular phase, ovulation, and a luteal phase. During the follicular phase, under the influence of FSH, one follicle becomes dominant by day 7. Estradiol, the main hormone promoting endometrial growth during this phase, reaches a peak shortly before the LH surge on day 14. The follicle ruptures within 12 hours of the LH surge and about 24 hours after the estradiol peak. After ovulation, estradiol levels plummet, and progesterone, produced by the corpus luteum, becomes the dominant hormone as the luteal phase starts. Progesterone inhibits the growth of a new follicle and causes maturation of the proliferative endometrium. In the absence of fertilization, the corpus luteum degenerates over the following 14 days at which time progesterone levels decline steeply. Progesterone withdrawal is responsible for initiation of bleeding during the normal menstrual cycle. The normal menstrual cycle lasts 2-7 days, occurs at intervals of 21-35 days, and leads to an average blood loss of 35-40 mL up to a maximum of 80 mL (see
Figure 76-1
).
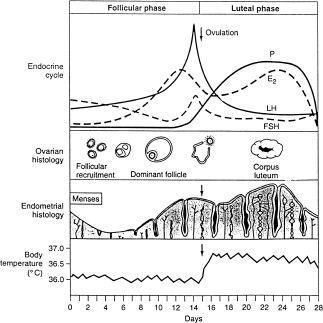
FIGURE 76-1.
The hormonal, ovarian, endomethal, and basal body temperature changes and relationships throughout the normal menstrual cycle. (Reproduced, with permission, from Carr BR, Wilson JD. Disorders of the ovary and female reproductive tract, in Isselbacher KJ, Braunwald E, Wilson JD, et al. Harrison’s Principles of Internal Medicine, 13th ed. New York: McGraw-Hill; 1998: 2101.)
3.
(B)
Polymenorrhea is defined as uterine bleeding at regular intervals of less than 21 days. Metrorrhagia is defined as uterine bleeding at irregular but frequent intervals. Menorrhagia and hypermenorrhea are synonymous and describe prolonged or excessive bleeding at regular intervals. Menometrorrhagia indicate prolonged or excessive bleeding at irregular intervals.
4.
(B)
Dysfunctional uterine bleeding is defined as heavy, prolonged unpatterned uterine bleeding unrelated to structural or organic disease. It results from anovulation and is responsible for 90% of abnormal vaginal bleeding in adolescents. In the absence of ovulation, there will not be progestins to allow for maturation and stabilization of the endometrium. Because of the effects of unopposed estrogen, the endometrium remains in a proliferative phase, becomes unstable, and bleeds erratically. Because dysfunctional uterine bleeding is a diagnosis of exclusion, a thorough history should be obtained to rule out organic causes, including complications of early pregnancy, coagulopathies, STDs, side effects of medications and drugs among others. Regardless of the etiology, in any patient complaining of abnormal vaginal bleeding it is essential to evaluate the severity of past and ongoing bleeding and to address any potential need for hospitalization, IV fluids, or blood replacement.
5.
(C)
Genital cancers, although included in the differential diagnosis, would be unlikely in a 17-year-old adolescent. Most cases of abnormal vaginal bleeding in adolescence are secondary to dysfunctional uterine bleeding. However, the differential diagnosis to consider includes
• Pregnancy-related conditions: intrauterine or ectopic pregnancy, spontaneous abortion, and molar-trophoblastic disease
• Infections: vaginitis, cervicitis, endometritis, salpingitis, and PID
• Other gynecologic conditions: ovarian cysts, genital cancers, breakthrough bleeding associated with contraceptive use, ovulation bleeding, and polyps
• Systemic diseases: renal and liver failure
• Blood dyscrasias
• Direct trauma and foreign body
• Medications: anticoagulants and platelet inhibitors
6.
(E)
A pelvic examination is rarely indicated in a postpubertal, not sexually active patient within 18 months of menarche unless trauma is suspected. All other women with abnormal vaginal bleeding should have a pelvic examination, particularly when there is a pattern of increasing, protracted or very heavy bleeding. Blood pressure and heart rate, both in the upright and supine position, would be essential to assess hemodynamic instability and potential need for hospitalization. A complete physical examination will be needed, documenting general appearance, pallor, tachycardia, abdominal masses, guarding, rebound, or evidence of endocrinopathies. Breasts should be checked for galactorrhea. Recent weight gain or loss may play a role in dysfunctional uterine bleeding. Moderate acne, particularly in a patient with obesity and hirsutism, suggests hyperandrogenism.
7.
(D)
A pregnancy test will be essential to exclude complications of pregnancy as the cause of abnormal vaginal bleeding. Hemoglobin and hematocrit determinations will help determine the magnitude of chronic bleeding. Coagulation studies may reveal coagulopathies or blood dyscrasias, such as in patients with a pattern of excessive bleeding since menarche and/or in patients with a family history of abnormal vaginal bleeding. Among adolescents requiring hospitalization for this problem, 20% have coagulopathies. Testing for infections will be needed in sexually active teens with abnormal bleeding because gonorrhea, chlamydia, and trichomonal infections are common causes of protracted or irregular vaginal bleeding in adolescents who previously had regular periods. Endocrine abnormalities such as hypothyroidism and polycystic ovarian syndrome frequently present with menorrhagia or irregular bleeding. Thyroid function tests, FSH and LH, prolactin, and androgen studies will help confirm these diagnoses. Endometrial biopsy is not indicated in adolescents.
8.
(A)
Numerous options are available for the treatment of patients with anovulatory, dysfunctional uterine bleeding. Patients with acute, very heavy, or uncontrolled bleeding should be hospitalized and treated with IV estrogen, 25 mg every 4 hours, until bleeding abates. If bleeding is less heavy and the patient is hemodynamically stable, conjugated estrogens orally can be given in the outpatient setting until bleeding stops at which time the dose of estrogens can be reduced to 1.25-2.5 mg/day and oral medroxyprogesterone acetate 10 mg orally added for 7-10 days. On discontinuing these medications, withdrawal bleeding will occur. Patients with acute moderate bleeding can be treated with combined oral contraceptives given up to 4 times a day with gradual tapering until bleeding subsides. At that time the patient should continue to take 1 pill a day until the pack is finished. In patients with significant anemia, taking only the pharmacologically active pills in each package for 21 days, discarding the placebo pills, and starting a new package will prevent withdrawal bleeding. This method of administration may be used for 2-3 cycles to promote a faster resolution of the anemia. Iron therapy should be offered to all patients to correct iron deficiency and prevent further anemia. In this patient, any of the listed outpatient hormonal treatments can be used. In view of her moderate bleeding, hemodynamic stability, and moderate anemia, hospitalization does not seem necessary at this time.
9.
(A)
Weight gain is rarely a side effect of the pill. Nausea and breakthrough bleeding, however, are among the most common. Both side effects tend to abate after the first few cycles. Nausea is considered an estrogenic side effect of the pill and, if bothersome, it can be corrected by choosing a pill with a lower estrogen content. Other potential side effects of the pill include headaches, breast tenderness, hypertension, abdominal cramping or bloating, and changes in menstrual flow.
10.
(E)
Typical use failure rates reflect the percentage of women experiencing an unintended pregnancy during the first year of use of the method under assessment. Injectable depomedroxyprogesterone has the lowest failure rate of all hormonal contraceptive methods (0.3%), although calcium supplementation needs to be taken daily to prevent bone density loss associated with long-term use. The Food and Drug Administration (FDA) recommends seeking alternative contraceptive methods after 2 years of use. Combined oral contraceptive pills have a typical use failure rate of 2% in the general population, but those rates are much higher (7-15%) in adolescent girls aged 15-19 years, mostly as a result of poor compliance. Progestin-only pills have a somewhat higher failure rate than combined pills. For male condoms the typical failure rate is 12%; for couples using no method the chance of pregnancy climbs to 85%.
11.
(E)
Combined oral contraceptives have a protective effect against endometrial and ovarian cancer. They also have some other beneficial effects, including regulation of menses, decreasing the severity of dysmenorrhea, reduced iron loss, improved bone mineralization, and lowered risk of ectopic pregnancy and symptomatic PID.
12.
(B)
Combined oral contraceptives can safely be used in all the conditions listed except active viral hepatitis in which it is absolutely contraindicated. Other absolute contraindications include
• Pregnancy
• Breast cancer
• Migraine headaches with focal neurologic signs
• Breastfeeding within 6 weeks postpartum
• Hypertension with systolic BP higher than 160 and diastolic BP higher than 100
• History of or current deep venous thrombosis or pulmonary embolism
• Vascular disease
• Major surgery with prolonged immobilization
• History of or current ischemic heart disease or stroke
• Complicated valvular heart disease
• Diabetic retinopathy, neuropathy, nephropathy
• Benign hepatic adenoma
Relative contraindications to the use of combined oral contraceptives include mild hypertension, sickle cell disease, depression, and migraine without focal neurologic findings.
13.
(B)
Rifampin is known to decrease the contraceptive effectiveness of the pill.
14.
(E)
Carbamazepine as well as most anticonvulsants, including phenytoin, ethosuximide, felbamate, and topiramate, decreases the contraceptive effects of the pill. All other medications listed increase estrogen levels and may lead to potential side effects such as nausea, vomiting, headaches, and breast tenderness.
15.
(D)
Combined oral contraceptives decrease the clearance of benzodiazepines, caffeine, theophylline, tricyclic antidepressants, and prednisolone, potentially increasing their risk for toxicity. However, aspirin and morphine concentrations may decrease in users of estrogen-progestin pills.
16.
(B)
IUDs are an excellent method of long-term reversible contraception for women and sometimes adolescent girls in long-term, mutually monogamous relationships, and have the lowest failure rate of all contraceptive methods, 0.1%. Newer evidence shows they are safe in nulliparous women, although in this situation there is a higher expulsion rate after insertion. They are generally not recommended for women with multiple sexual partners, high risk for STDs, heavy or painful menstrual periods, or those with cervical dysplasia. In addition, IUDs have one of the highest continuation rates versus other contraception choices. The transdermal contraceptive patch (Ortho Evra; failure rate 0.3%) and the vaginal ring (NuvaRing; failure rate 0.3%) share all the indications and contraindications of the birth control pill but may be more convenient for teens because they do not require daily compliance on the part of the user. The “patch” needs to be replaced once a week; the vaginal ring, which delivers an estrogenprogestin combination absorbed through the vaginal mucosa, is replaced monthly. Medroxyprogesterone injections (failure rate 0.3%) constitute another method with a low failure rate. However, it should not be used for more than 2 years due to the potential decrease in bone mineral density, even if the patient is taking the recommended daily calcium supplementation. Diaphragms and cervical caps have high failure rates (20% and 40%, respectively).
