Pediatric Examination and Board Review (79 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

Fox VL. Gastrointestinal bleeding in infancy and childhood.
Gastroenterol Clin North Am.
2000;29(1):37-66.
Heikenen JB, Pohl JF, Werlin SL, et al. Octreotide in pediatric patients.
J Pediatr Gastroenterol Nutr.
2002;35(5):600-609.
Hyer W, Beveridge I, Domizio P, et al. Clinic management and genetics of gastrointestinal polyps in children.
J Pediatr Gastroenterol Nutr.
2000;31(5):467-479.
CASE 49: A 6-WEEK-OLD WITH VOMITING
A 6-week-old boy comes to your office with several days of vomiting and irritability. He vomits “everything he eats.” The vomiting does not have any blood in it and is not associated with diarrhea or fever. The vomitus is described as being light in color but not green or yellow. The baby was born at full term with no complications. His birthweight was 3.2 kg.
On physical examination this is a well-nourished child: the weight is 4.4 kg, the HR is 180, and the RR is 38. His anterior fontanel is slightly sunken and there are dry mucous membranes. The abdomen is nondistended with normal bowel sounds. The remainder of the examination is unremarkable.
Laboratory studies-serum
Sodium (Na) 135 mEq/mL
Chloride (Cl) 99 mEq/mL
Potassium (K) 4.0 mEq/mL
Bicarbonate (HCO
3
) 30 mEq/mL
SELECT THE ONE BEST ANSWER
1.
This child’s diagnosis most likely is
(A) GERD
(B) malrotation
(C) pyloric stenosis
(D) viral gastroenteritis
(E) urea cycle defect
2.
The diagnostic test to confirm this diagnosis is
(A) pH probe
(B) upper GI series
(C) ultrasound of the abdomen
(D) serum NH
3
(E) the diagnosis should be made on clinical grounds, and no further testing is necessary
3.
If the laboratory investigation and physical examination were normal, the most likely diagnosis would be
(A) GERD
(B) malrotation
(C) pyloric stenosis
(D) viral gastroenteritis
(E) urea cycle disorder
4.
The diagnostic test to confirm the condition in question 3 is
(A) pH probe
(B) upper GI series
(C) ultrasound of the abdomen
(D) upper endoscopy
(E) this is a diagnosis made on clinical grounds; no further testing is necessary
5.
The first-line treatment for GERD includes
(A) surgery
(B) thickened feeds
(C) antacid medication
(D) change the infant’s formula
(E) B and C
6.
If the child in the opening vignette had bilious vomiting, the most likely diagnosis would be
(A) duodenal atresia
(B) intestinal malrotation
(C) pyloric stenosis
(D) Hirschsprung disease
(E) intracranial hemorrhage
7.
The least helpful diagnostic test you could use to confirm the condition in question 6 is
(A) abdominal radiograph
(B) barium enema
(C) upper GI series
(D) ultrasound
(E) CT
8.
The true statement about Ladd bands is
(A) Ladd bands obstruct the duodenum
(B) Ladd bands can originate from the duodenum
(C) Ladds bands are peritoneal bands that can be associated with an annular pancreas
(D) Ladd bands can originate in the hepatic flexure
(E) all of the above
9.
If the child in question 6 was 6 hours old and had Down syndrome, the likely diagnosis would be
(A) GERD
(B) malrotation
(C) duodenal atresia
(D) Hirschsprung disease
(E) atrioventricular (AV) canal malformation and heart failure
10.
The diagnostic test you would order in this instance is
(A) abdominal radiograph
(B) upper GI series
(C) barium enema
(D) pH probe
(E) echocardiogram
11.
When you go back and review this child’s prenatal ultrasound, you would likely see
(A) oligohydramnios
(B) the renal agenesis associated with this syndrome
(C) polyhydramnios
(D) hepatomegaly
(E) no consistent intrauterine finding
12.
If the 6-hour-old infant with vomiting had a normal radiograph and a normal upper GI series but had a serum glucose of 20 mg/dL, your first step would be
(A) start ranitidine for the reflux
(B) start IV fluids with antibiotics
(C) encourage more oral feeds for hypoglycemia
(D) give IV glucose
(E) recheck the serum glucose
13.
If the patient is a 2-year-old with vomiting and minimal abdominal pain who has normal vital signs, an Na of 130 mEq/mL and a HCO
3
of 15 mEq/mL, the diagnosis is likely
(A) viral gastroenteritis
(B) malrotation
(C) GERD
(D) cyclic vomiting
(E) pancreatitis
14.
Despite giving the patient in question 13 a fluid bolus, correcting the abnormal laboratory studies, and improving the vital signs, the child continues to vomit. Your next step is
(A) prochlorperazine suppository
(B) IV H
2
blocker
(C) IV ondansetron
(D) promethazine suppository
(E) upper GI series to rule out malrotation
15.
The 2-year-old in question 13 has intermittent, severe cramping abdominal pain without diarrhea and between episodes has no symptoms. To make the diagnosis you need a
(A) blood culture
(B) upper GI series
(C) barium enema
(D) renal ultrasound
(E) CT of the abdomen
16.
The 2-year-old vomits several times in the morning with no abdominal pain and has a normal physical examination. The remainder of the day he has no GI symptoms but is fussy. The likely diagnosis is
(A) GERD
(B) hydronephrosis
(C) intermittent volvulus
(D) brain tumor
(E) cyclic vomiting
17.
The child in question 16 has 1 episode of “coffee ground” emesis. What is your concern?
(A) she needs more aggressive antacid therapy
(B) she needs endoscopy to rule out malignancy
(C) she needs an upper GI series because she likely has a malrotation
(D) A and C
(E) A, B, and C
18.
The child in question 16 is noted to have weight loss, poor appetite, and a poor balance. Your first concern is which of the following?
(A) she needs more aggressive antacid therapy
(B) she needs a renal ultrasound
(C) she needs an upper GI series
(D) she needs a CT scan of the brain
(E) toxic ingestion
ANSWERS
1.
(C)
Pyloric stenosis is a thickening of the pylorus muscle. A patient usually becomes symptomatic after 3 weeks of age. It is characterized by nonbilious vomiting and hypochloremic alkalosis (see
Figure 49-1
).
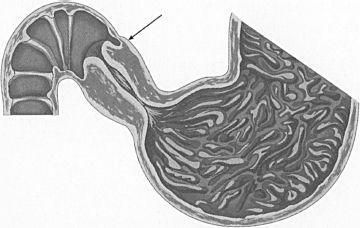
FIGURE 49-1.
Hypertrophic pyloric stenosis. Note that the distal end of the hypertrophic muscle protrudes into the duodenum (arrow), accounting for the ease of perforation into the duodenum during pyloromyotomy. (Reproduced, with permission, from Doherty G. Current Diagnosis & Treatment: Surgery, 13th ed. New York: McGraw-Hill; 2010: Fig. 43-9.)
2.
(C)
The diagnosis of pyloric stenosis may be confirmed by palpation of the thickened pylorus on physical examination. The pylorus will be a firm, mobile olive-shaped mass. However, this is very difficult to palpate, and the diagnosis is usually confirmed on ultrasound. Although changes will be seen on an upper GI series, it has increased risk compared with ultrasound and is therefore not considered the best diagnostic test.
3.
(A)
GERD is the most common diagnosis for a healthy child with nonbilious vomiting. In a patient with severe viral gastroenteritis you would not expect normal vital signs, without fever or diarrhea.
