Pediatric Examination and Board Review (81 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(D) the inheritance is autosomal recessive; only symptomatic patients need to be treated so no screening is necessary
(E) is caused by sporadic mutations and therefore there are never other family members affected by the disease
7.
If the patient’s ANA titer is 1:640 and the anti-smooth muscle antibody is 1:320, the patient’s diagnosis is
(A) type 1 autoimmune hepatitis
(B) type 2 autoimmune hepatitis
(C) type 3 autoimmune hepatitis
(D) all of the above
(E) none of the above
8.
The treatment for autoimmune hepatitis would include
(A) steroids
(B) ganciclovir
(C) lamivudine
(D) all of the above
(E) there is no effective medical treatment; referral to a transplant center is required
9.
If the symptoms of the patient in the initial vignette were due to hepatitis B, the infection would be
(A) acute hepatitis B
(B) congenitally acquired chronic hepatitis B
(C) unknown because you need a hepatitis B surface antigen to be able to distinguish between acute and chronic infection
(D) unknown because you need a quantitative hepatitis B DNA level to distinguish between acute and chronic infection
(E) unknown because without further history, you cannot distinguish what type of hepatitis B infection the patient has
10.
Had the patient in the vignette presented with a small firm liver, splenomegaly, and ascites, the disease that created these symptoms could have been any of the following, except
(A) hepatitis B
(B) Wilson disease
(C) type 1 autoimmune hepatitis
(D) hepatitis A
(E) hepatitis C
11.
While you are awaiting the lab results in a jaundiced child, the patient’s mother calls to say she is “difficult to wake up.” Your next step is
(A) repeat her liver numbers
(B) see her in your office before repeating the labs
(C) increase her fluid intake because her lethargy is likely secondary to dehydration
(D) refer her to an emergency department for evaluation
(E) admit her and observe
12.
Fulminant hepatic failure is defined as
(A) a patient with liver disease who develops encephalopathy and coagulopathy
(B) a patient with liver disease who develops encephalopathy
(C) a patient without preexisting liver disease who develops encephalopathy and coagulopathy within 8 weeks of the onset of liver disease
(D) a patient without preexisting liver disease who develops encephalopathy within 16 weeks of the onset of liver disease
(E) a patient without preexisting liver disease who develops coagulopathy within 16 weeks of the onset of liver disease
13.
The problems that arise in children with fulminant hepatic failure include
(A) hypoglycemia
(B) coagulopathy
(C) renal failure
(D) encephalopathy
(E) all of the above
14.
If the child in the initial vignette had been ill for several days with viral upper respiratory infection (URI) symptoms, which additional laboratory study would you order?
(A) adenovirus culture
(B) acetaminophen level
(C) enterovirus culture
(D) influenza A culture
(E) all of the above
15.
If the acetaminophen level was high, the likelihood of successfully treating the patient’s toxicity is
(A) less likely than an asymptomatic patient
(B) more likely than an asymptomatic patient
(C) equivalent to an asymptomatic patient
(D) there are no data to predict the chance of successful treatment
(E) there is no known treatment for acetaminophen toxicity
16.
Suppose the child was 2 years old and had RUQ pain and an enlarged liver. Suppose further that she was anicteric and the hepatitis A serology was negative. In this instance, the next step would be
(A) ultrasound and an alpha-fetoprotein level
(B) hepatitis B and C serology
(C) α
1
-antitrypsin level, ceruloplasmin
(D) ANA, anti-smooth muscle antibody, anti-liver kidney microsomal antibody determinations
(E) all of the above
17.
The likely diagnosis for that patient is
(A) hepatocellular carcinoma
(B) hepatoblastoma
(C) rhabdosarcoma
(D) angiosarcoma
(E) metastatic disease from another primary tumor
18.
If a young child (2-8 years old) had a sudden onset of RUQ pain, fever, and jaundice, the likely diagnosis would be
(A) cholecystitis
(B) choledochal cyst
(C) sclerosing cholangitis
(D) cholangiocarcinoma
(E) liver hematoma
ANSWERS
1.
(A)
A child with RUQ pain and jaundice must be assumed to have some form of hepatitis. Hepatitis A causes 50% of acute hepatitis in the United States. Transmission is via person to person or by water- and foodborne outbreaks. In utero maternal-child transmission has not been recognized. The incubation period is about 4 weeks. Most children have vague symptoms: low-grade fever, nausea, vomiting, and hepatomegaly. The vast majority of young children are anicteric. The disease is self-limited in the great majority of cases. Young children can have anicteric hepatitis A.
2.
(A)
See above explanation. Acute Epstein-Barr virus (EBV) infections frequently cause hepatomegaly but almost always there are other associated symptoms (fever, lymphadenopathy, sore throat, fatigue, and splenomegaly). Patients with hepatitis B infection are jaundiced.
3.
(E)
Table 50-1
lists the differential diagnosis and the appropriate tests required.
TABLE 50-1.
Differential Diagnosis of Jaundice in the Older Child
| DISEASE | DIAGNOSTIC TEST |
α | α |
Wilson disease | Ceruloplasmin, urine copper, dry weight of copper in liver |
Type 1 autoimmune hepatitis | ANA, anti-smooth muscle antibody |
Type 2 autoimmune hepatitis | Anti-liver kidney microsomal antibody |
Hepatitis B | Hepatitis B surface antigen |
Hepatitis C | Hepatitis C antibody |
4.
(B)
The pathophysiology of Wilson disease is an inability to mobilize copper from lysosomes within the hepatocytes. When the liver has reached its storage capacity, the copper escapes and begins to damage other organ systems. There is an increase in urinary copper. There are neuropsychological symptoms, renal disease, and hemolysis. Copper is needed but not available for production of ceruloplasmin. Therefore the level is low.
5.
(A)
See above explanation.
6.
(B)
Wilson disease has an autosomal recessive inheritance. Patients are more effectively treated before symptoms occur; therefore all family members should be screened for asymptomatic disease.
7.
(A)
Type 1 autoimmune hepatitis is associated with a positive ANA and anti-smooth muscle antibody. Type 2 autoimmune hepatitis is associated with anti-liver and kidney microsomal antibodies. There is no type 3.
8.
(A)
The treatment for autoimmune hepatitis is steroids and azathioprine. Once the liver numbers have returned to the normal range, the initial high dose of steroids can be weaned. There is no infectious etiology known for the disease; therefore antivirals (ganciclovir and lamivudine) would not be appropriate.
9.
(B)
Hepatitis B is transmitted by the percutaneous route, use of IV drugs, sexual contact, or in utero maternal-child transmission. There are reports of household contact spread, but because hepatitis B vaccination is part of routine pediatric care it is less likely she would be infected from a household contact. An 8-year-old is likely to have acquired the infection from mother at birth. This child would therefore have a chronic infection. See
Table 50-2
to interpret the markers, which distinguish acute from chronic infection.
10.
(D)
The description here is of cirrhosis with evidence of portal hypertension, secondary to chronic liver disease. Although hepatitis A can rarely cause fulminant hepatic failure, it does not have a chronic form. The other listed diseases do.
11.
(D)
A child who is jaundiced and then is “difficult to wake up” must be assumed to have encephalopathy. This should be evaluated in an emergency department where laboratory evaluations and treatment are immediately available.
12.
(C)
13.
(E)
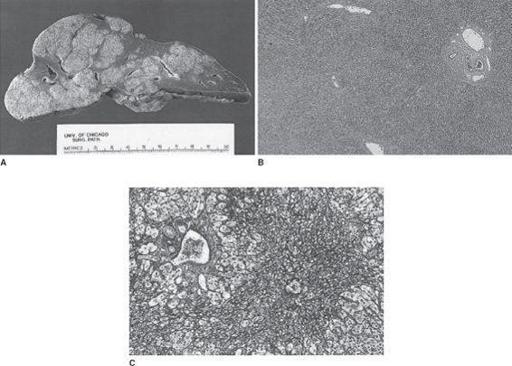
Patients with fulminant hepatic failure (FHF) have a decreased liver mass. They are at risk for hypoglycemia secondary to decreased glycogen storage and gluconeogenesis. Such a patient may develop hepatorenal syndrome. The mechanism is unknown, but the disease is characterized by decreased excretion of Na (as opposed to acute tubular necrosis where Na excretion is increased). Coagulopathy develops because the liver produces factors I (fibrinogen), II, V, VII, IX, and X. In addition in FHF there is frequently DIC contributing to the coagulopathy that may be difficult to control. Encephalopathy is characteristic of hepatic failure (see
Figure 50-1
).
TABLE 50-2.
Serum Markers in Hepatitis B Infections
| HBsAg | HBsAb | HBc Igm | HBc IgG | HBeAg | HBeAb | HB DNA | |
| Early acute | + | − | + | − | + | − | + |
| Late acute | + | − | + | − | − | + | + |
| Chronic | + | − | − | + | + | − | + |