Pediatric Examination and Board Review (80 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

4.
(E)
GERD is a clinical diagnosis. Although pH probes and endoscopy can be used to document changes consistent with reflux, neither is needed to confirm the diagnosis.
5.
(B)
The first-line treatments for reflux are conservative changes. These include limiting the volume the baby consumes per feed, positioning the baby upright after feeds, and thickening the child’s formula with 1 tablespoon of rice cereal per ounce. Infants who fail these measures should then undergo antacid therapy.
6.
(B)
Bilious vomiting is indicative of distal obstruction. The most common cause of obstruction in this age group is an intestinal malrotation (see
Figure 49-2
).

FIGURE 49-2.
Abdominal radiograph of a 10-day-old infant with bilious emesis. Note the dilated proximal bowel and the paucity of distal bowel gas, characteristic of a volvulus. (Reproduced, with permission, from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery, 9th ed. New York: McGraw-Hill; 2010: Fig. 39-16.)
7.
(A)
In a malrotation, the duodenal jejunal loop is on the right side of the abdomen. The cecum is on the left side instead of the right. The malrotation occurs around the superior mesenteric vessel, and the superior mesenteric vein lies to the left of the artery instead of to the right. A barium enema can be used to locate the cecum, and an upper GI series can be used to visualize the duodenum. An ultrasound can be used to locate the superior mesenteric vessel. The least helpful test is a plain radiograph because a normal exam does
not
obviate the need for another imaging study (see
Figure 49-3
).
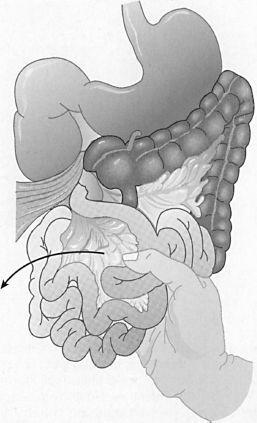
FIGURE 49-3.
Malrotation of the midgut with volvulus. Note cecum at the origin of the superior mesenteric vessels. Fibrous bands cross and obstruct the duodenum as they adhere to the cecum. Volvulus is untwisted in a counterclockwise direction. (Reproduced, with permission, from Doherty G. Current Diagnosis & Treatment: Surgery, 13th ed. New York: McGrawHill; 2010: Fig. 43-11.)
8.
(A)
Ladd bands are peritoneal bands that come from the malrotated cecum to the RUQ and can cause duodenal obstruction.
9.
(C)
Duodenal atresia is apparent in the first 24 hours of life. Thirty percent of children with duodenal atresia have Down syndrome.
10.
(A)
Abdominal radiograph will demonstrate the “double bubble” sign. There is gas in the stomach and the proximal duodenum but no gas in the distal bowel.
11.
(C)
The amniotic fluid produced cannot travel through a gut with an atresia. Therefore there is an excess (polyhydramnios) of fluid. Fifty percent of children with esophageal and duodenal atresia have polyhydramnios.
12.
(D)
Although the likely cause of hypoglycemia and vomiting is sepsis and further evaluation is indicated, it is imperative that the hypoglycemia be corrected immediately.
13.
(A)
14.
(C)
Ondansetron is a serotonin 5-HT
3
receptor antagonist with excellent antiemetic effects. When given in the emergency department, ondansetron decreases vomiting and the need for hospital admission.
15.
(C)
The signs described are likely those of an intussusception but could be due to a malrotation with intermittent volvulus. A contrast enema could be used to diagnose either condition. If an upper GI study is performed and no diagnosis is made, the performance of a contrast enema may be delayed because of residual contrast material moving through the small bowel and interfering with the interpretation of the contrast enema.
16.
(A)
Although morning vomiting is concerning because of its association with central nervous system (CNS) pathology, in a patient with a normal physical examination and no other symptoms, the diagnosis is likely GERD.
17.
(A)
GI bleeding in this patient is likely secondary to peptic acid disease. GI malignancy in this age group is rare. Malrotation would be associated with abdominal pain and likely bilious emesis.
18.
(D)
Morning vomiting is concerning. In a patient who is having neurologic signs, not eating a normal diet, and losing weight, you must be concerned about a brain tumor.
 S
S
UGGESTED
R
EADING
Colleti RB, DiLorenzo C. Overview of pediatric gastroesophageal reflux disease and proton pump inhibitor therapy.
J Pediatr Gastroenterol Nutr.
2003;37(suppl 1):7-11.
Maclennan AC. Investigations in vomiting children.
Semin Pediatr Surg.
2003;12(4):220-228.
Reeves JJ, Shannon MW, Fleisher GR. Ondansetron decreases vomiting associated with acute gastroenteritis: a randomized controlled study.
Pediatrics.
2002;109(4):e62.
CASE 50: AN 8-YEAR-OLD WITH JAUNDICE
An 8-year-old girl presents to your office with a 3-day history of decreased appetite and abdominal pain. She denies fever or diarrhea but has nausea and intermittent vomiting.
Physical examination reveals a jaundiced girl with a height and weight at the 50th percentile for age. The abdomen is soft and nondistended with positive bowel sounds, but the patient has diffuse RUQ pain and an enlarged liver without splenomegaly.
SELECT THE ONE BEST ANSWER
1.
The most appropriate first test is
(A) hepatitis A antibody
(B) monospot test
(C) hepatitis B surface antigen
(D) hepatitis C antibody
(E) all of the above
2.
If the patient in the vignette had not been jaundiced, your initial evaluation would include
(A) hepatitis A antibody
(B) monospot
(C) hepatitis B surface antigen
(D) hepatitis C antibody
(E) all of the above
3.
If the hepatitis A serology is negative, the next step in your evaluation of this 8-year-old jaundiced child is
(A) hepatic function panel, PT, GGTP
(B) α
1
-antitrypsin level, ceruloplasmin
(C) anti-smooth muscle antibody, antinuclear antibody (ANA), anti-liver and kidney microsomal antibodies
(D) hepatitis B antigen, hepatitis C antibody
(E) all of the above
4.
In Wilson disease
(A) serum ceruloplasmin is increased and the urinary copper is increased
(B) serum ceruloplasmin is decreased and the urinary copper is increased
(C) serum ceruloplasmin is increased and the urinary copper is decreased
(D) serum ceruloplasmin is decreased and the urinary copper is decreased
(E) normal serum ceruloplasmin level but increased urinary copper
5.
Suppose the ceruloplasmin level is consistent with Wilson disease. Left untreated, the other organ system(s) most likely to be affected includes
(A) neuropsychiatric
(B) cardiac
(C) respiratory
(D) all of the above
(E) none of the above
6.
In Wilson disease
(A) the inheritance is autosomal dominant and all family members should be screened for asymptomatic disease
(B) the inheritance is autosomal recessive and all family members should be screened for asymptomatic disease
(C) the inheritance is autosomal dominant; only symptomatic patients need to be treated so no screening is necessary
