Pediatric Examination and Board Review (91 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

A 4-year-old boy comes to your office because of ear pain. It began the night before and woke him from sleep several times. Appropriate doses of analgesics for the pain did not help much. His mother reports temperatures as high as 102°F (38.8°C). He had a cold approximately 1 week ago that has been improving the last several days.
On examination he is afebrile. His nares have scant, clear rhinorrhea; the oropharynx is normal. His right TM and ear canal appear normal. His left ear canal is normal, but the TM is bulging outward and is light yellow with erythema around the rim. His lungs are clear to auscultation.
SELECT THE ONE BEST ANSWER
1.
Which of the following is the least likely pathogen associated with his ear pain?
(A)
Haemophilus influenzae
(B)
Streptococcus pneumoniae
(C) influenza virus
(D)
Moraxella catarrhalis
(E) chlamydia
2.
Which of the following is/are risk factors for this problem?
(A) craniofacial abnormality
(B) exposure to cigarette smoke
(C) formula use
(D) gastroesophageal reflux
(E) all of the above
3.
Besides direct observation of the TM, which of the following methods is/are helpful to diagnose otitis media?
(A) tympanogram
(B) radiographs of the skull
(C) pure tone audiometry
(D) pneumatic otoscopy
(E) A and D
4.
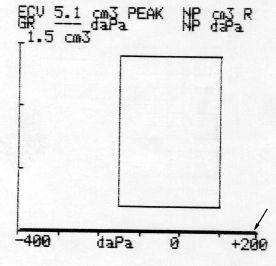
Which of the following tympanograms would you expect with this patient?
(A) completely flat; high on the y-axis (high volume)
(B) rounded or somewhat flattened peak
(C) sharp peak at 0 daPa
(D) completely flat; low on the y
-
axis
(E) none of the above
5.
All of the following are complications of otitis media except
(A) mastoiditis
(B) pneumonia
(C) brain abscess
(D) meningitis
(E) facial palsy
6.
If you choose to put him on an antibiotic, which is your
first
choice?
(A) azithromycin
(B) amoxicillin-clavulanic acid
(C) ciprofloxacin ear drops
(D) ceftriaxone
(E) amoxicillin
7.
If he returned 3 days later because of no change in his symptoms and his examination was exactly the same, what would your next step be?
(A) tympanocentesis
(B) tympanogram
(C) change the oral antibiotic
(D) add oral steroids
(E) add topical ear drops
8.
In which of the following scenarios would you choose observation over antibiotic treatment?
(A) a 4-year-old with purulent effusion, limited TM mobility, minimal pain, no fever or other systemic symptoms
(B) a 6-week-old with same findings as above
(C) a 3-year-old with purulent effusion, limited TM mobility, and severe otalgia
(D) all of the above
(E) none of the above
9.
If you had begun a patient with unilateral AOM on antibiotic therapy and he returned 1 week later, still on medication, with a new otitis media on the other side, which is your next course of action?
(A) tympanocentesis
(B) tympanogram
(C) change antibiotic
(D) add oral steroids
(E) add topical ear drops
10.
His mother calls you worried 2 days later because he has a very high fever, 103°F (39.4°C) axillary, and it appears that his “ear is bulging outward.” What is his likely diagnosis?
(A) otitis media with perforation
(B) subdural abscess
(C) acute mastoiditis
(D) meningitis
(E) foreign body
11.
Of the following choices, what is the next best action for the case in question 10?
(A) admission for additional evaluation and intravenous (IV) antibiotics
(B) change to a stronger oral antibiotic
(C) tympanostomy tubes
(D) biopsy of mastoid
(E) course of oral steroids
12.
Which of the following is
not
an indication for tympanocentesis?
(A) otitis media in an immune-compromised patient
(B) AOM and temperature of 102.6°F (39.2°C) in a 3-week-old
(C) mastoiditis
(D) a 2-month history of clear effusion with some conductive hearing loss
(E) failure of second-line treatment of AOM
13.
You see a 2-year-old child in your office for a checkup and note on examination a clear effusion with air-fluid levels behind his left TM, which is mobile on pneumatic otoscopy. He has no ear pain, fever, or other symptoms. What is your diagnosis?
(A) otitis media
(B) recurrent otitis media
(C) resistant otitis media
(D) otitis media with effusion
(E) chronic serous otitis media
14.
You see the 2-year-old from question 13 back in your office 3 months later with the same physical findings and still no symptoms. His parents note that he seems to say “what?” a lot when they are talking to him. What is your next action?
(A) no testing
(B) audiology referral for hearing test
(C) antibiotics
(D) speech therapy
(E) tympanostomy tubes
15.
You see an 8-year-old for ear pain that she has had for 4 days. She had a cold last week, but most of the congestion and cough has resolved. She has had no fevers, no drainage from the ear, and analgesics help the pain minimally. On examination her TM appears retracted, and your in-office tympanogram shows a flattened peak between 200 and 0 daPa. What is her diagnosis?
(A) otitis externa
(B) otitis media
(C) otitis media with effusion
(D) eustachian tube dysfunction
(E) cholesteatoma
16.
A 3-year-old girl with bilateral tympanostomy tube placement 6 months ago comes to you with purulent discharge from her left ear for 1 day. She has had a temperature of 102°F (38.8°C) in the last day and is eating less than her usual amount. She has no other symptoms. What is the best management of this patient?
(A) amoxicillin
(B) amoxicillin/clavulanic acid
(C) topical fluoroquinolone drops
(D) topical steroid and fluoroquinolone drops
(E) oral steroids
17.
What is the least likely pathogen involved in chronic suppurative otitis?
(A)
P aeruginosa
(B)
S aureus
(C)
Escherichia coli
(D)
Proteus mirabilis
(E)
S pneumoniae
18.
All of the following are possible treatments and managements for chronic suppurative otitis media except
(A) surgical intervention
(B) topical antibiotics
(C) close observation
(D) oral antibiotics
(E) hearing evaluation
ANSWERS
1.
(E)
Tympanocentesis studies have revealed the etiology of otitis media to be
S pneumoniae
in 20-35% of cases,
H influenzae
in 20-30%,
Moraxella catarrhalis
in 20%, no isolate in 20-30%, and a virus in 17-44%.
Chlamydia
species are not believed to be common causes of AOM, although in several studies
Chlamydia
species have been identified by tympanocentesis culture in children with otitis media with effusion.
2.
(E)
Smoking, reflux, and craniofacial abnormalities, especially cleft lip, put children at increased risk for AOM (children with cleft lip have recurrent otitis media). Multiple studies have shown that infants fed formula have a higher rate of otitis media than breast-fed infants. This difference likely reflects both the protective effect of breast milk and the predisposition to otitis media when bottles of formula milk are “propped up.”
3.
(E)
Radiographs have no role in diagnosing otitis media, and a hearing test may indeed be abnormal but will not help the practitioner distinguish among AOM, otitis media with effusion, or other forms of conductive hearing loss. Pneumatic otoscopy is the best single sign correlating with post-TM effusion.
4.
(B)
Tympanograms estimate air pressure and volume of the middle ear space. The normal pressure, or compliance, of a healthy TM fluctuates from −200 to +200 daPa when a tone, sound energy, is applied to it. A graph is produced with air pressure on the x
-
axis and volume on the y
-
axis. A tympanogram of a normal middle ear space should have a high peak at atmospheric pressure (0 on the graph) (see
Figure 56-1
). With middle ear effusion of any cause, there is some mobility of the TM, but it is dampened, producing a rounded curve instead of a sharp peak and often a more negative middle ear pressure.
With eustachian tube dysfunction (most commonly secondary to a cold or sinusitis), there is negative pressure in the middle ear space compared with the nasopharynx, and so middle ear pressures are in the more extreme negative range, −400 to −200 daPa. With a perforated TM, the ear canal and the middle ear are at the same pressure, so that applying a force to the ear canal produces a flat tracing, often with high volume (higher on the
y
curve).
5.
(B)
Mastoiditis, brain abscess, and meningitis are all possible complications of AOM, either through direct extension or hematogenous spread. Facial nerve palsy occurs because of the proximity of the facial nerve to the middle ear.