Pediatric Examination and Board Review (92 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

FIGURE 56-1.
Tympanogram of otitis media. The compliance tracing of an ear with otitis media. The line is flat (arrow). (Reproduced, with permission, from Knoop KJ, Stack LB, Storrow AS, et al. Atlas of Emergency Medicine, 3rd ed. New York: McGraw-Hill; 2010:98. Photo contributor: Lawrence B. Stack, MD.)
6.
(E)
Despite recognized resistance of the major otitis pathogens to penicillin, amoxicillin is still the first choice for treatment. Low-dose amoxicillin (45 mg/kg per day) is no longer preferred and a higher dose (90 mg/kg per day) should be instituted. Amoxicillin-clavulanic acid should be reserved for resistant or recurrent otitis media that has been clinically refractory to high-dose amoxicillin. Cephalosporins, either ceftriaxone intramuscularly (IM) for 3 days or an oral second- or third-generation drug, should be reserved for penicillin-allergic patients, as should azithromycin. Antimicrobial ear drops play no role in the management of AOM, unless there is a perforation in the TM, in which case recent studies have shown similar benefit with antibiotic- and steroid-containing drops versus oral amoxicillin alone.
7.
(C)
After beginning antibiotic therapy for AOM, resolution of symptoms should begin within 24-48 hours. In this case, it is appropriate to try a different antibiotic because one-fourth of
S pneumoniae
isolates are resistant to penicillin, and one-fourth to one-third of
H influenzae
isolates are ampicillin resistant (beta-lactamase positive). All
Moraxella
species are resistant because of beta-lactamase production. Tympanocentesis may be helpful in guiding a change in therapy but is not the first step. A tympanogram will not provide any extra knowledge. Steroids have no role in the management of otitis media.
8.
(A)
The most recent guidelines for management of AOM recommend observation for children with uncomplicated otitis media—the absence of high fever or severe pain. Otitis media occurring in a 6-week-old child always requires treatment, followup, and, sometimes, further workup.
9.
(C)
In this case after asking about compliance, it is also appropriate to try a different antibiotic regimen with a broader antimicrobial spectrum, for the same reasons as in answer 7.
10.
(C)
This is the clinical picture of acute mastoiditis, which can be a complication of otitis media. Causative organisms are usually
S pneumoniae
,
S pyogenes
,
S aureus
,
Pseudomonas
species, and
H influenzae
. Sixty percent of mastoiditis occurs in children younger than 2 years. Clinical findings include fever, point tenderness, and fluctuance over the mastoid, prominence of the pinna, and usually otitis media. Incidentally, all cases of uncomplicated AOM by virtue of proximity show some inflammation of the mastoid air cells. Beyond that, when the infection spreads to the overlying periosteum but
not
the underlying bone, the diagnosis is acute mastoiditis (see
Figure 56-2
). Spread to the underlying bone constitutes acute mastoid osteitis, a case that may require medical and surgical management.
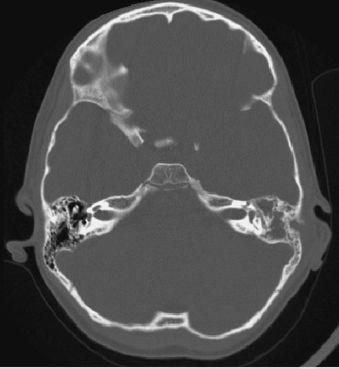
FIGURE 56-2.
Acute mastoiditis. Axial CT image shows an acute fluid collection within the mastoid air cells on the left. (Reproduced, with permission, from Fauci AS, Kasper DL, Braunwald E, et al. Harrison’s Principles of Internal Medicine, 17th ed. New York: McGraw-Hill; 2008: Fig. 31-1.)
11.
(A)
All cases of suspected mastoiditis should be confirmed by CT of the temporal bone to distinguish acute mastoiditis from mastoid osteitis. For acute mastoiditis, myringotomy and parenteral antibiotics are the next steps.
12.
(D)
Otitis media in young infants who have systemic symptoms should warrant tympanocentesis as part of the sepsis workup. Two months of clear effusion is otitis media with effusion and does not require tympanocentesis in this time frame.
13.
(D)
Because of the lack of purulent fluid, outward bulging of the TM, and the presence of a freely mobile TM, all other possible answers are excluded.
14.
(B)
Otitis media with effusion is considered “persistent” when it has been present for 3 months or more. By that time, if no resolution or improvement is seen, a hearing test is the next appropriate step, especially if subjective hearing loss is still evident and not resolving. A conductive hearing loss would likely be found.
15.
(D)
Eustachian tube dysfunction is common in the weeks following an upper respiratory infection (URI). The only finding on examination is a retracted TM, and symptomatically the child may complain of frequent popping, pain, or pressure. Various over-the-counter (OTC) remedies have been employed to treat this, including pseudoephedrine and nasal saline sprays.
16.
(A)
Recent studies have proven that topical otic drops that are a combination of antibiotics and steroids are equivalent if not superior in eradicating otitis media with tympanostomy tubes. However, use of quinolones in this fashion encourages antimicrobial resistance and should be therefore avoided.
17.
(A)
P aeruginosa
in the absence of a perforated eardrum and otorrhea is a rare cause of otitis media.
18.
(C)
Surgery may be required if there is an anatomic defect that is acting as a continued bacterial medium (ie, cholesteatoma). Observation is not an acceptable treatment plan because hearing loss often ensues with chronic otitis media and worsens with time.
 S
S
UGGESTED
R
EADING
Behrman RE, Kliegman RM, Jenson HB, et al.
Nelson Textbook of Pediatrics
. Philadelphia, PA: WB Saunders; 2007.
Hendley JO. Otitis media.
N Engl J Med.
2002;347:1169-1174.
CASE 57: A 14-YEAR-OLD BOY WITH A SORE THROAT AND ENLARGED SPLEEN
A 14-year-old boy comes into your office complaining of sore throat of 1 week’s duration. It is getting worse by the day, and this morning he felt as if he could not swallow his breakfast, both because of the pain on swallowing and because it felt as if something was “blocking it down there.” He has been feeling hot and cold but has not measured his temperature. He is feeling fatigued, but the rest of his review of systems is negative. He has had multiple episodes of “tonsillitis” this year.
On examination, he is cooperative but appears quite tired. His temperature is 101.5°F (38.6°C) orally; the other vital signs are normal. His conjunctivae are clear, TMs are normal, and oropharynx is quite erythematous with enlarged erythematous tonsils covered by diffuse white exudates bilaterally. No petechiae are seen. His lymphatic examination reveals anterior and posterior cervical lymphadenopathy, all 1-2.5 cm in diameter, mobile, and moderately tender. His lungs are clear. The cardiovascular examination is normal, and the abdominal examination reveals a palpable spleen tip 4 cm under the rib cage. There is no rash.
SELECT THE ONE BEST ANSWER
1.
What is his most likely diagnosis?
(A) streptococcal pharyngitis
(B) viral upper respiratory tract infection
(C) adenoviral pharyngotonsillitis
(D) mononucleosis
(E) peritonsillar abscess
2.
What kind of microorganism most likely caused this infection?
(A) gram-positive coccus
(B) enterovirus
(C) herpesvirus
(D) echovirus
(E) Coxsackie virus
3.
Which of the following is
not
a clinical association of this patient’s likely diagnosis?
(A) Guillain-Barré syndrome
(B) maculopapular dermatitis
(C) pharyngoconjunctival fever
(D) transient thrombocytopenic purpura
(E) bilateral orchitis
4.
During what time of year is this illness most common?
(A) spring
(B) summer
(C) fall
(D) winter
(E) no seasonal association
5.
What is the incubation period of this illness?
(A) 1-4 days
(B) 4-7 days
(C) 7-14 days
(D) 14-28 days
(E) 30-50 days
6.
What is the best specimen to diagnose this disease?
(A) sputum
(B) oropharyngeal secretions
(C) blood
(D) urine
