Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (104 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

Management
(
Lancet
2009;373:659;
Ann Rheum Dis
2010;69:631)
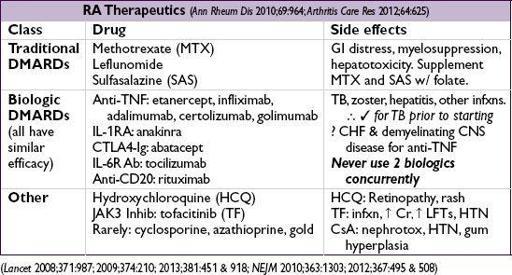
• Early dx and Rx (esp. DMARD) w/ frequent follow-up and escalation of Rx as needed to
achieve clinical remission
or low disease activity • ↓ time to remission ↑ length of sustained remission (
↑ length of sustained remission (
Arthritis Res Ther
2010;12:R97) • Sero- disease (eg, RF or anti-CCP) a/w aggressive joint disease & EAM
disease (eg, RF or anti-CCP) a/w aggressive joint disease & EAM
• Start
both
rapid acting agent (to acutely ↓ inflammation) and
D
isease
-M
odifying
A
nti
-R
heumatic
D
rug
(DMARD)
(typically take 1–3 mo to have max effect) at dx • Rapid-acting drugs:
NSAIDs
or COX-2 inhibitors (↑ CV adverse events);
glucocorticoids
[low-dose (<20 mg/d oral) or joint injection]; or
NSAIDs + glucocorticoids: ↑ GI adverse events, minimize long-term concurrent use
•
DMARDs
MTX
(1st line unless CKD, hepatitis, EtOH or lung disease), SAS or leflunomide; consider HCQ if seronegative and mild disease;
if inadequate response after 3 mo (despite DMARD dose escalation):
combination Rx
w/ other traditional DMARDs (ie, MTX, SAS and HCQ) or
biologic
(anti-TNF typically 1st line unless contraindication)
• Given ↑ r/o early CV morbidity/mortality, ↓ risk w/ lifestyle mgmt, lipid & DM screening
ADULT ONSET STILL’S DISEASE & RELAPSING POLYCHONDRITIS
Adult onset Still’s disease
(
Drugs 2008;68:319)
•
Rare autoinflammatory synd
;=
w/ typical onset 16–35 y; sx evolve over wks to mos • Dx if 5 criteria are present & ≥2 major; exclude infxn, malig, other rheumatic, drug rxn
major
: fever ≥39°C for ≥1 wk (usually daily or twice daily high-spiking fever); arthralgias/arthritis ≥2 wk; Still’s rash (qv); ↑ WBC w/ 80% PMN
minor
: sore throat; LAN; HSM; ↑ AST/ALT/LDH; negative ANA & RF
• Still’s rash (>85%): nonpruritic macular or maculopapular salmon-colored rash; usually trunk or extremities; may be precipitated by trauma (Koebner phenomenon), warm water • Plain films: soft tissue swelling (
early
) → cartilage loss, erosions, carpal ankylosis (
late
) • Treatment: NSAIDs, steroids; steroid-sparing: MTX,
anakinra
, anti-TNF, tocilizumab • Variable clinical course: 20% w/ long-term remission; 30% remit-relapse; ~50% chronic (esp. arthritis); ↑ risk of macrophage activation syndrome (life-threatening)
Relapsing polychondritis
(
Autoimmun Rev
2010;9:540)
• Inflammatory destruction of cartilaginous structures; onset usually age 40–60 y,=
• Subacute onset of
red
,
painful
and
swollen cartilage
; ultimately atrophic & deformed • Common clinical features: bilateral auricular chondritis; nonerosive inflammatory arthritis; nasal chondritis; ocular inflammation; laryngeal or tracheal chondritis; cochlear and/or vestibular dysfxn • 40% of cases a/w immunologic disorder (eg, RA, SLE, vasc., Sjögren’s), cancer or MDS
• Clinical diagnosis based on exam with multiple sites of cartilaginous inflammation
• Labs: ↑ ESR & CRP, leukocytosis, eosinophilia, anemia of chronic inflammation
• Bx (not req for dx): proteoglycan depletion, perichondrial inflammation and replacement with granulation tissue and fibrosis; immunofluorescence with Ig and C3 deposits • Screen for pulm (PFTs, CXR/CT, ± bronch) and cardiac (ECG, TTE) involvement
• Therapy guided by disease activity and severity:
steroids
1st line; NSAIDs, dapsone for sx control of arthralgias and mild disease; MTX or AZA for steroid-sparing; cyclophosphamide for organ-threatening disease
CRYSTAL DEPOSITION ARTHRITIDES
GOUT
Definition & epidemiology
(
Lancet
2010;375:318;
NEJM
2011;364:443)
• Humans lack enzyme to metabolize urate (end-product of purine metabolism) • Monosodium urate (MSU) crystal deposition in joints promotes inflammation • >
> (9:1); peak incidence 5th decade; most common cause of inflammatory arthritis in
(9:1); peak incidence 5th decade; most common cause of inflammatory arthritis in over 30 y; rare in premenopausal
over 30 y; rare in premenopausal (estrogens promote renal urate excretion)
(estrogens promote renal urate excretion)