Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (108 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

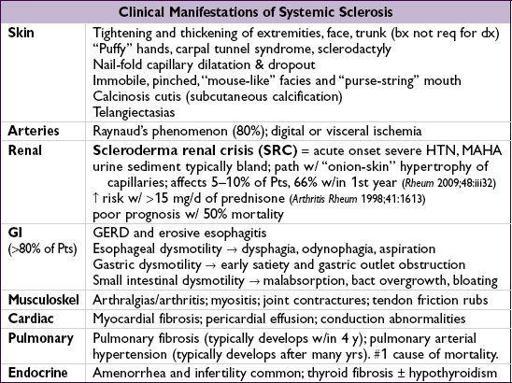
SYSTEMIC SCLEROSIS AND SCLERODERMA DISORDERS
Definition & epidemiology
(
Best Pract Res Clin Rheumatol
2010;24:857)
•
Scleroderma
refers to the presence of tight, thickened skin •
Localized scleroderma
: morphea (plaques of fibrotic skin), linear (fibrotic bands), “en coup de saber” (linear scleroderma on one side of scalp and forehead saber scar) •
saber scar) •
Systemic sclerosis (SSc)
=scleroderma + internal organ involvement. Subgroups:
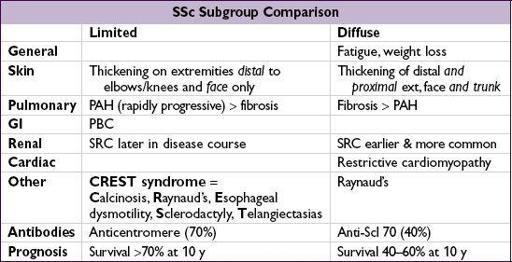
SSc w/ limited cutaneous disease
SSc w/ diffuse cutaneous disease: rapidly progressive disorder affecting skin
SSc sine scleroderma (visceral disease without skin involvement, rare)
• Peak onset of SSc between
ages 30–50
;>
(7:1); African American > white • 1–2/100,000 annual incidence of systemic disease in the U.S.
• Pathogenesis: immune damage to endothelial cells and reactive O
2
species production → persistent oxidative stress → perivascular inflammation → fibroblast activation and fibrosis. Cytokines, growth factors, genetics, environmental factors and autoantibodies (against PDGF receptor, endothelial cells and fibroblasts) all contribute (NEJM 2009;360:1989).
Classification criteria
(1 major or 2 minor; 97% Se, 98% Sp; Arth Rheum 1980;23:581)
• Major:
skin findings extend
proximal
to MCP or MTP joints
• Minor:
sclerodactyly
(skin findings limited to the fingers)
digital pitting scars
from loss of substance on the finger pad
bibasilar
pulmonary fibrosis
•
Other causes
of thickened skin: diabetes (scleredema ≠ scleroderma), hypothyroidism, nephrogenic systemic fibrosis, eosinophilic fasciitis, amyloidosis, GVHD, drug or toxin
Diagnostic studies & monitoring
• Autoantibodies
anti-Scl-70
(antitopoisomerase 1): 40% of diffuse, 15% of limited; ↑ risk pulm fibrosis
anticentromere
: 60–80% of limited, <5% of diffuse, ↑ risk of severe digit ischemia
ANA (>90%),
RF (30%),
anti-RNP a/w overlap syndrome
• At baseline: ✓ BUN/Cr & UA for proteinuria, PFTs (spirometry, lung volumes, D
L
CO), high-res chest CT (if diffuse disease), TTE (RVSP for PHT), RHC if ↑ RVSP or suspect PHT
• Annual PFTs; TTE q1–2y • Skin bx not routine, but helpful to assess other possible causes for skin thickening • ↑ r/o malignancy at affected sites
Treatment
(
Ann Rheum Dis
2009;68:620)
• Pulmonary Fibrosis:
cyclophosphamide
(NEJM 2006;354:2655), steroids
PAH: pulmonary
vasodilators
(see “Pulm Hypertension”), early Rx a/w better outcomes
• Renal: monitor BP monthly, intervene early to avoid HTN crisis; dipstick for protein
Scleroderma renal crisis:
ACE inhibitors
(not ARB); ACEi not indicated for prophylaxis
• GI: PPI and/or H2-blockers for GERD; antibiotics for malabsorption
hypomotility: metoclopramide or erythromycin; nonoperative Rx of pseudo-obstruction
• Cardiac: NSAIDs or steroids for pericarditis • Arthritis: acetaminophen, NSAIDs, hydroxychloroquine, PT
• Myositis: MTX, AZA, steroids • Skin: PUVA for morphea. For pruritus: emollients, topical or oral steroids (↓ dose). Immunosuppressives offer only minimal to modest benefit for skin fibrosis.