Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (52 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.63Mb size Format: txt, pdf, ePub
Clinical manifestations
• May be asx; biliary pain in
2%/y; once sx, rate of complications
2%/y •
Biliary pain (“colic”)
=
episodic RUQ or epigastric abd pain
that begins abruptly, is continuous, resolves slowly and lasts for 30 min–3 h; ± radiation to scapula; nausea •
May be precipitated by fatty foods
• Physical exam: afebrile, ± RUQ tenderness or epigastric pain
Diagnostic studies
• RUQ U/S: Se & Sp >95% for stones >5 mm; can show complications (cholecystitis); should be performed only after fasting ≥8 h to ensure distended, bile-filled gallbladder
Treatment
• Cholecystectomy (CCY), usually laparoscopic, if symptomatic
• CCY in asx Pts w/: GB calcification (~7% risk of ca) (
Surgery
2001;129:699), GB polyps >10 mm, Native American, stones >3 cm or bariatric surgery or cardiac transplant candidates • Ursodeoxycholic acid (rare) for cholesterol stones w/ uncomplicated biliary pain or if poor surgical candidate; also reduces risk of gallstone formation with rapid wt loss • Biliary pain: NSAIDs (eg, diclofenac 50 mg IM) drug of choice, efficacyopiates & ↓ complications (
Aliment Pharmacol Ther
2012;35:1370)
Complications
• Cholecystitis: 20% of sx biliary pain → cholecystitis w/in 2 y
• Choledocholithiasis → cholangitis or gallstone pancreatitis
• Mirizzi’s syndrome: common hepatic duct compression by cystic duct stone → jaundice, biliary obstruction • Cholecystenteric fistula: stone erodes through gallbladder into bowel
• Gallstone ileus: SBO (usually at term ileum) due to stone in intestine that passed thru fistula • Gallbladder carcinoma (~1% in U.S.)
CHOLECYSTITIS (
NEJM
2008;358:2804)
Pathogenesis
• Acute cholecystitis: stone impaction in cystic duct → inflammation behind obstruction → GB swelling ± secondary infection (50%) of biliary fluid
• Acalculous cholecystitis: gallbladder stasis and ischemia → inflammatory response; occurs mainly in critically ill, hosp. Pts (postop major surgery, TPN, sepsis, trauma, burns, opiates, immunosuppression, infxn [eg, CMV,
Crypto, Campylobacter
, typhoid fever])
Clinical manifestations
• History: RUQ/epigastric pain ± radiation to R shoulder/back, nausea, vomiting, fever
•
Physical exam: RUQ tenderness
, Murphy’s sign = ↑ RUQ pain and inspiratory arrest with deep breath during palpation of R subcostal region, ± palpable gallbladder
• Laboratory evaluation: ↑ WBC, ± mild ↑ bilirubin, AΦ, ALT/AST and amylase; AST/ALT >500 U/L, bili >4 mg/dL or amylase >1000 U/L → choledocholithiasis
Diagnostic studies
•
RUQ U/S
: high Se & Sp for stones, but need
specific signs of cholecystitis
: GB wall thickening >4 mm, pericholecystic fluid and a sonographic Murphy’s sign
•
HIDA scan
: most Se test (80–90%) for acute cholecystitis. IV inj of HIDA (selectively secreted into biliary tree). In acute cholecystitis, HIDA enters BD but not GB. 10–20% false(cystic duct obstructed from chronic cholecystitis, lengthy fasting, liver disease).
Treatment
• NPO, IV fluids, nasogastric tube if intractable vomiting, analgesia
•
Antibiotics
(
E. coli
,
Klebsiella
and
Enterobacter
sp. are usual pathogens) ([2nd-or 3rd-generation cephalosporin or FQ] + MNZ) or piperacillin-tazobactam
• Early CCY (usually w/in 72 h). Delaying surgery 2–3 mo ↓ operative time w/o Δ rate of complications or conversion to open procedure (
Am J Surg
2008;194:40).
• If unstable for surgery, EUS-guided transmural or ERCP-guided transcystic duct drainage is equivalent to cholecystostomy (
Gastro
2012;142:805)
• Intraoperative cholangiogram or ERCP to r/o choledocholithiasis in Pts w/ jaundice, cholangitis or stone in BD on U/S
Complications
• Gangrenous cholecystitis: necrosis w/ risk of empyema and perforation
• Emphysematous cholecystitis: infection by gas-forming organisms (air in GB wall)
• Post CCY: bile duct leak, BD injury or retained stones, cystic duct remnant, sphincter of Oddi dysfxn
CHOLEDOCHOLITHIASIS
Definition
• Gallstone lodged in bile duct (BD)
Epidemiology
• Occurs in 15% of Pts w/ gallbladder stones; can form de novo in BD
Clinical manifestations
• Asymptomatic (50%)
• RUQ/epigastric pain due to obstruction of bile flow → ↑ BD pressure, jaundice, pruritus, nausea
Diagnostic studies
• Labs: ↑ bilirubin, AΦ; transient spike in ALT or amylase suggests passage of stone • RUQ U/S: BD stones seen ~50% of cases; usually inferred from dilated BD (>6 mm) • ERCP preferred dx modality when likelihood high; cholangiogram (percutaneous, operative) when ERCP unavailable or unsuccessful; EUS/MRCP to exclude BD stones when suspicion low
Treatment
• ERCP & papillotomy w/ stone extraction (± lithotripsy)
• CCY typically w/in 6 wk unless contraindication (>15% Pts will develop indication for CCY if left unRx’d)
Complications
• Cholangitis, cholecystitis, pancreatitis, stricture
CHOLANGITIS
Definition & etiologies
• BD obstruction → infection proximal to the obstruction
•
Etiologies: BD stone
(~85%)
Malignant (biliary, pancreatic) or benign stricture
Infection w/ fluke (
Clonorchis sinensis
,
Opisthorchis viverrini
)
Clinical manifestations
• Charcot’s triad: RUQ pain, jaundice, fever/chills; present in ~70% of Pts • Reynolds’ pentad: Charcot’s triad + shock and Δ MS; present in ~15% of Pts
Diagnostic studies
• RUQ U/S
• Labs: ↑ WBC, bilirubin, AΦ, amylase;BCx • ERCP; percutaneous transhepatic cholangiogram (if ERCP unsuccessful)
Treatment
•
Antibiotics
(broad spectrum) to cover common bile pathogens (see above) ampicillin + gentamicin (or levofloxacin) ± MNZ (if severe); carbapenems; pip/tazo • ~80% respond to conservative Rx and abx → biliary drainage on elective basis •
~20% require urgent biliary decompression
via ERCP (papillotomy, stone extraction and/or stent insertion). If sphincterotomy cannot be performed (larger stones), decompression by biliary stent or nasobiliary catheter can be done; otherwise percutaneous transhepatic biliary drainage or surgery.
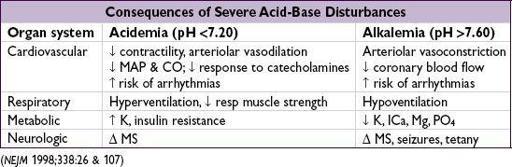
ACID-BASE DISTURBANCES
GENERAL
Definitions
•
Acidemia
→ pH <7.36,
alkalemia
→ pH >7.44
•
Acidosis
→ process that increases [H+];
alkalosis
→ process that decreases [H+]
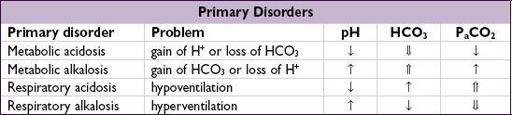
• Primary disorders: metabolic acidosis or alkalosis, respiratory acidosis or alkalosis
• Compensation
respiratory: hyper-or hypoventilation alters P
a
CO
2
to counteract 1° metabolic process renal: excretion/retention of H+/HCO
3
to counteract 1° respiratory process respiratory compensation occurs in minutes; renal compensation takes hours to days
compensation never fully corrects pH;
if pH normal, consider mixed disorder
Workup
• Determine
primary disorder
: ✓ pH, P
a
CO
2
, HCO
3
• Determine if
degree of compensation
is appropriate
Other books
French Lessons by Georgia Harries
Amanda Scott by Highland Secrets
Bound by Lust by Shanna Germain
A Lost Kitten by Kong, Jessica
Flinch Factor, The by Michael Kahn
Algoma by Dani Couture
Shadows Return by Lynn Flewelling
Me encontrarás en el fin del mundo by Nicolas Barreau
Clever Girl by Tessa Hadley