Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (55 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

• Lung parenchyma abnormalities (often cause hypoxia → ↑ RR → resp. alk., but eventual muscle fatigue → resp. acid.): pneumonia, pulmonary edema, restrictive lung disease
• Thoracic cage abnormalities: pneumothorax, flail chest, kyphoscoliosis
• Post infusion of bicarbonate in acidemic Pt w/ limited ability to ↑ minute ventilation
RESPIRATORY ALKALOSIS
Etiologies
(
NEJM
2002;347:43)
•
Hypoxia
→
hyperventilation
: pneumonia, pulm. edema, PE, restrictive lung disease •
Primary hyperventilation
CNS stimulation, pain, anxiety, fever, trauma, stroke, voluntary
drugs: salicylates, progesterone, methylxanthines, nicotine pregnancy, sepsis, hepatic failure
•
Pseudorespiratory alkalosis
: ↓ perfusion w/ preserved ventilation (eg, CPR, severe HoTN) → ↓ delivery of CO
2
to lungs for excretion; low P
a
CO
2
but ↑ tissue CO
2
SODIUM AND WATER HOMEOSTASIS
OVERVIEW
General
• Disorders of serum sodium are generally due to Ds in
total body water
, not sodium • Hyper-or hypo-osmolality → rapid water shifts → Ds in brain cell volume → Δ MS, seizures
Key hormones
•
Antidiuretic hormone (ADH)
: primary hormone that regulates
sodium concentration
stimuli for secretion: hyperosmolality, ↓↓ effective arterial volume (EAV), angiotensin II action: insertion of aquaporin-2 channels in collecting ducts → passive water reabsorption
urine osmolality
is an indirect functional assay of the ADH-renal axis U
osm
range: 60 mOsm/L (no ADH) to 1200 mOsm/L (maximal ADH) •
Aldosterone
: primary hormone that regulates
total body sodium
(and ∴ volume) stimuli for secretion: hypovolemia (via renin and angiotensin II), hyperkalemia action: iso-osmotic reabsorption of sodium in exchange for potassium or H
+
HYPONATREMIA
Pathophysiology
•
Excess of water relative to sodium
; almost always due to ↑
ADH
• ↑ ADH may be
appropriate
(eg, hypovolemia or hypervolemia with ↓ EAV) • ↑ ADH may be
inappropriate
(SIADH) • Rarely, ↓ ADH (appropriately suppressed), but kidneys unable to maintain nl [Na]
serum
1
°
polydipsia:
ingestion of massive quantities (usually >12 L/d) of free H
2
O overwhelms diluting ability of kidney (normal dietary solute load ~750 mOsm/d, minimum U
osm
= 60 mOsm/L → excrete in ~12 L; if H
2
O ingestion exceeds this amount → H
2
O retention)
“tea & toast
” and
“beer potomania”
: ↓↓ daily solute load, ↑ free H
2
O → insufficient solute to excrete H
2
O intake (eg, if only 250 mOsm/d, minimum U
osm
= 60 mOsm/L → excrete in ~4 L; if H
2
O ingestion exceeds this amount → H
2
O retention)
Workup
(
NEJM
2000;342:1581;
JASN
2012;23:1140)
•
History
: (1) acute vs. chronic (>48 h); (2) sx severity; (3) risk for neuro complications (alcoholism, malnourished, cirrhosis, older females on thiazides, hypoxia, hypoK) • Measure
plasma osmolality
Hypotonic hyponatremia
most common scenario; true excess of free H
2
O relative to Na
Hypertonic hyponatremia:
excess of another effective osmole (eg, glc, mannitol) that draws H
2
O intravascularly; each 100 mg/dL ↑ glc >100 mg/dL → ↓ [Na] by 2.4 mEq/L
Isotonic hyponatremia:
rare lab artifact from hyperlipidemia or hyperproteinemia
• For hypotonic hyponatremia, ✓
volume status
(vital signs, orthostatics, JVP, skin turgor, mucous membranes, peripheral edema, BUN, Cr, uric acid) •
U
osm
diagnostically useful in limited circumstances, because almost always >300 exceptions: U
osm
<100 in 1° polydipsia & ↓ solute intake moreover, U
osm
>300 ≠ SIADH; must determine if ↑ ADH appropriate or inappropriate however, U
osm
important when deciding on
treatment
(see below) • If euvolemic and ↑ U
osm
, evaluate for glucocorticoid insufficiency and hypothyroidism
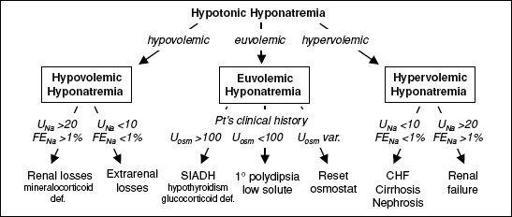
Figure 4-4 Approach to hyponatremia
Hypovolemic hypotonic hyponatremia
(ie, ↓↓ total body Na, ↓ TBW)
•
Renal losses
(U
Na
>20 mEq/L, FE
Na
>1%): diuretics (esp. thiazides, as loop diuretics
↓ tonicity of medullary interstitium and impair urine concentrating ability), salt-wasting nephropathy, cerebral salt wasting, mineralocorticoid deficiency
•
Extrarenal losses
(U
Na
<10 mEq/L, FE
Na
<1%): GI losses (eg, diarrhea), third-spacing (eg, pancreatitis), inadequate intake, insensible losses
Euvolemic hypotonic hyponatremia
(ie, ↑ TBW relative to total body Na)
•
SIADH
(eu-or mild hypervolemia, inapprop ↑ U
Osm
,
normal U
Na
, ↓ BUN & UA)
malignancy
: lung, brain, GI, GU, lymphoma, leukemia, thymoma, mesothelioma
pulmonary
: pneumonia, TB, aspergillosis, asthma, COPD, PTX,pressure ventilation
intracranial
: trauma, stroke, hemorrhage, infxn, hydrocephalus, Guillan-Barré syndrome
drugs
: antipsychotics, antidepressants (esp.
SSRIs
), chemotherapy, AVP, MDMA
miscellaneous
: pain, nausea, postoperative state
•
Endocrinopathies
: ↑ ADH activity seen in
glucocorticoid deficiency
(co-secretion of ADH & CRH) and
severe
hypothyroidism/myxedema coma
(↓ CO & ↓ GFR) •
Psychogenic polydipsia
(U
osm
<100, ↓ uric acid): usually requires intake >12 L/d •
Low solute
(↓ U
Na
, ↓ U
osm
) “tea & toast”; “beer potomania”
• Reset osmostat: chronic malnutrition (↓ intracellular osmoles) or pregnancy (hormonal effects) → ADH physiology reset to regulate a lower [Na]
serum
Hypervolemic hypotonic hyponatremia
(ie, ↑ total body Na, ↑ ↑ TBW)
•
CHF
(↓ CO → ↓ EAV; U
Na
<10 mEq/L, FE
Na
<1%) •
Cirrhosis
(splanchnic arterial vasodilation + ascites → ↓ EAV; U
Na
<10 mEq/L, FE
Na
<1%) •
Nephrotic syndrome
(hypoalbuminemia → edema → ↓ EAV; U
Na
<10 mEq/L, FE
Na
<1%) •
Advanced renal failure
(diminished ability to excrete free H
2
O; U
Na
>20 mEq/L)
Treatment
(
Curr Opin Nephrol Hypertens
2010;19:493)
•
Approach
: depends on
volume status
,
acuity
of hypoNa, and if
symptomatic
Asx or chronic symptomatic: correct [Na]
serum
at rate of ≤0.5 mEq/L/h
Acute sx:
initial
rapid correction of Na (2 mEq/L/h for the first 2–3 h) until sx resolve
Rate of ↑ Na
should not exceed 6
(chronic) to
8
(acute) mEq/L/d to avoid central pontine myelinolysis
/
osmotic demyelination syn. (CPM/ODS: paraplegia, dysarthria, dysphagia)
•
Frequent lab draws
and
IVF rate adjustments
are cornerstones of treatment •
Overly rapid correction
: can lead to CPM/ODS. Should be emergently reversed w/ dDAVP ± D
5
W; partial neurologic recovery possible (
CJASN
2008;3:331) •
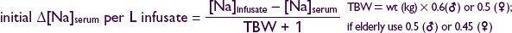
Effect of IV fluids
(
http://www.medcalc.com/sodium.html
)