Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (57 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

central DI: desmopressin (dDAVP)
nephrogenic DI: treat underlying cause if possible; Na restriction + thiazide (mild volume depletion → ↓ delivery of filtrate to dysfxnal diluting segment of kidney), consider amiloride for lithium-induced DI (
Kid Int
2009;76:44)
pregnancy-induced DI: due to vasopressinase from placenta, ∴ Rx w/ dDAVP
POTASSIUM HOMEOSTASIS
Overview
(
Annals
2009;150:619)
• Renal: potassium excretion regulated at
distal nephron
(collecting tubule) distal Na delivery & urine flow: Na absorption → lumen electronegative → K secretion metabolic alkalemia and aldosterone: increase Na absorption and K secretion • Transcellular shifts: most common cause of acute change in serum potassium Acid-base disturbance: K+/H+ exchange across cell membranes Insulin → stimulates Na-K ATPase → hypokalemia (mitigates postprandial ↑ K) Catecholamines → stimulate Na-K ATPase → hypokalemia; reversed by b-blockers Digoxin → blocks Na-K ATPase → hyperkalemia Massive necrosis (eg, tumor lysis, rhabdo, ischemic bowel) → release of intracellular K Hypo-or hyperkalemic periodic paralysis: rare disorders due to channel mutations • Diet: alone rarely causes ↑ or ↓ K (total body store
3500 mEq, daily intake
100 mEq)
HYPOKALEMIA
Transcellular shifts
• Alkalemia, insulin, catecholamines, hypokalemic/thyrotoxic periodic paralysis, acute ↑ in hematopoiesis (megaloblastic anemia Rx w/ B
12
, AML crisis), hypothermia, chloroquine, barium/cesium intoxication, antipsychotic overdose (risperidone, quetiapine)
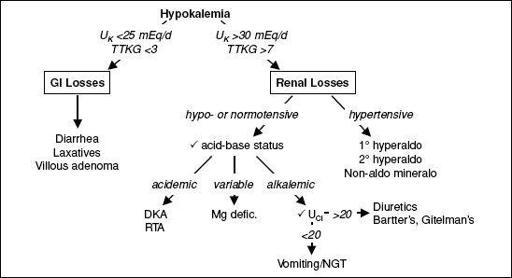
GI potassium losses
(U
K
<25 mEq/d or <5 mEq/L or TTKG <3)
• GI losses
plus
metabolic acidosis: diarrhea, laxative abuse, villous adenoma • Vomiting & NGT drainage usually manifest as
renal losses
due to 2° hyperaldo & met. alk.
Renal potassium losses
(U
K
>30 mEq/d or >
15 mEq/L or TTKG >7)
• Hypotensive or normotensive acidosis: DKA, RTA [proximal RTA (type II) and some distal RTAs (type I)] alkalosis: diuretics, vomiting/NGT drainage (via 2° hyperaldosteronism) Bartter’s syndrome (loop of Henle dysfxn → furosemide-like effect;
NEJM
1999;340:1177)
Gitelman’s syndrome (distal convoluted tubule dysfxn → thiazide-like effect)
↓ Mg: ? release Mg-mediated inhib. of ROMK channel ∴ ↑ K secretion (
JASN
2007;18:2649)
• Hypertensive: mineralocorticoid excess
1° hyperaldosteronism (eg, Conn’s syndrome, glucocorticoid-remediable aldosteronism)
2° hyperaldosteronism (eg, renovascular disease, renin-secreting tumor)
nonaldosterone mineralocorticoid (eg, Cushing’s, Liddle’s, exogenous mineralocort., licorice, congenital adrenal hyperplasia)
Clinical manifestations
• Nausea, vomiting, ileus, weakness, muscle cramps, rhabdomyolysis, polyuria • ECG: U waves, ± ↑ QT interval, ventricular ectopy (PVCs, VT, VF)
Workup
(
NEJM
1998;339:451)
• Rule-out transcellular shifts • ✓ 24-h
U
K
and
transtubular potassium gradient
(TTKG) = (U
K
/P
K
) / (U
osm
/P
osm
)
U
K
>30 mEq/d or >15 mEq/L or TTKG >7 → renal loss
U
K
<25 mEq/d or <15 mEq/L or TTKG <3 → extrarenal loss
• If renal losses, ✓
BP
,
acid-base
,
U
Cl
(U
Na
unreliable for volume status w/ alkalemia)
Figure 4-7
Approach to hypokalemia
Treatment
•
If true potassium deficit:
potassium repletion
(↓ 1 mEq/L200 mEq total body loss) KCl 40 mEq PO q4–6h if nonurgent, KCl 10 mEq/h IV if urgent, recheck K freq • Beware of excessive potassium repletion if transcellular shift cause of hypokalemia • Treat underlying cause (if hydration needed, avoid dextrose-containing solutions as dextrose → ↑ insulin → intracellular potassium shifts) • Replete low Mg: IV Mg-SO
4
1–2 g q2h (oral Mg-oxide poorly tolerated b/c diarrhea) Causes of low Mg: GI loss (diarrhea, bypass, pancreatitis, malnutrition, PPI); renal loss (diuretics, nephrotoxic drugs, EtOH, ↑ Ca, 1° wasting syndromes, volume expansion)
HYPERKALEMIA
Transcellular shifts
(
BMJ
2009;339:1019)
• Acidemia, insulin defic. (DM), b-blockers, dig intox., massive cellular necrosis (tumorlysis, rhabdo, ischem. bowel, hemolysis), hyperkalemic periodic paralysis, succinylcholine
Decreased GFR
• Any cause of oliguric or anuric AKI or any cause of end stage renal disease
Normal GFR but with Ø renal K excretion
• Normal aldosterone function
↓ EAV (K excretion limited by ↓
distal Na delivery & urine flow
): CHF, cirrhosis excessive K intake: in conjunction with impairment in K excretion or transcellular shift ureterojejunostomy (absorption of urinary K in jejunum)
•
Hypoaldosteronism
: same as etiologies of hypoaldo RTA (type IV)
↓ renin: diabetic nephropathy, NSAIDs, chronic interstitial nephritis, HIV normal renin, ↓ aldo synthesis: 1° adrenal disorders, ACEI, ARBs, heparin
↓ response to aldosterone meds: K-sparing diuretics, TMP-SMX, pentamidine, calcineurin inhibitors tubulointerstitial disease: sickle cell, SLE, amyloid, diabetes
Clinical manifestations
• Weakness, nausea, paresthesias, palpitations • ECG: peaked T waves, ↑ PR interval, ↑ QRS width, loss of P wave, sine wave pattern, PEA/VF (ECG: low sensitivity, cardiac arrest can be first electrical manifestation!)
Workup
(
Crit Care Med
2008;36:3246)
• Rule out pseudohyperkalemia (IVF with K, hemolysis during venipuncture, ↑ plt or WBC) • Rule out transcellular shift •
Assess GFR
, if normal: Consider ↓ distal Na delivery and urine flow
✓ transtubular K gradient (TTKG) = (U
K
/P
K
)/(U
osm
/P
osm
) <6 c/w hypoaldo (
JASN
2008;19:424)
•
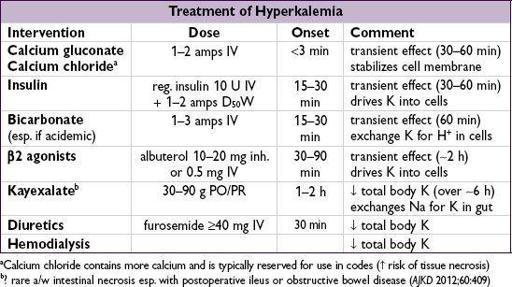
Rate of onset
important to note when establishing a treatment plan • Calcium helps prevent/treat cardiac complications; ∴ should be initial Rx, esp. if ECG Ds • Insulin, bicarbonate (esp. if acidemic), and b2 agonists should follow to ↓ plasma K
• Treatments that
eliminate total body K essential
as other Rxs will wear off with time; Kayexalate ± diuretics may be effective in many cases, but emergent hemodialysis should be considered in life-threatening situations • Patient information for diet education:
http://www.kidney.org/atoz/content/potassium.cfm
RENAL FAILURE
ACUTE KIDNEY INJURY (AKI)
Definition
(
CJASN
2008;3:844;
KI Suppl
2012;2:19)
• AKI: abrupt (<48 h) ↑ Cr ≥0.3 mg/dL, ↑ Cr ≥50%, or UOP <0.5 mL/kg/h for ≥6 h additional gradations based on further ↑ Cr & ↓ UOP, but not used clinically •
Cannot
estimate GFR using Cr in setting of AKI or D’ing Cr (requires steady state)
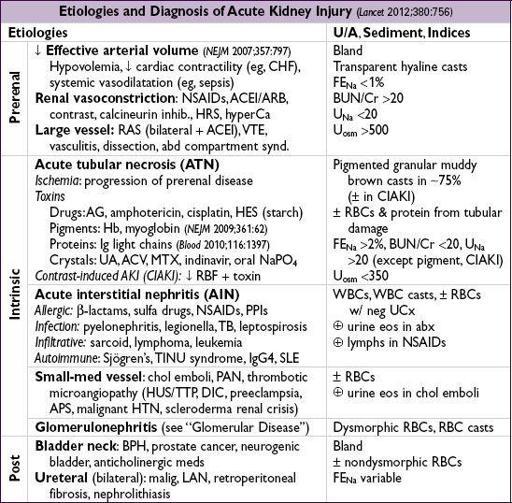
Workup
(
Lancet
2012;380:756)
•
H&P
: recent procedures & meds; thirst; VS & vol status; s/s of obstruction, vasc or systemic dis.; ischemia (prerenal & ATN) accounts for >50% of in-hospital AKI •
Urine evaluation
: output, urinalysis,
sediment
, electrolytes, and osmolality •
Fractional excretion of sodium (FE
Na
)
= (U
Na
/P
Na
)/(U
Cr
/P
Cr
)
<1% → prerenal, contrast, HRS or glomerulonephritis; >2% → ATN In setting of diuretics, ✓ FE
UN
= (U
UN
/P
UN
)/(U
Cr
/P
Cr
); <35% → prerenal
• Renal U/S or CT: r/o obstruction & eval kidney size to estimate chronicity of kidney disease • Serologies (if indicated): see “Glomerular Disease”
• Renal bx: may be necessary if cause remains unclear (esp if hematuria and/or proteinuria)