Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (98 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

•
Nonaldosterone mineralocorticoid excess
mimics hyperaldosteronism
11β-HSD deficiency (→ lack of inactivation of cortisol, which binds to nonselective mineralocorticoid receptor)
Black licorice (glycyrrhizinic acid inhibits 11β-HSD), extreme hypercortisolism (overwhelming 11β-HSD), exogenous mineralocorticoids
Liddle’s syndrome (constitutively activated/overexpressed distal tubular renal Na channel)
Clinical manifestations
•
Mild to moderate HTN
(11% of Pts w/ HTN refractory to 3 drugs;
Lancet
2008;371:1921), headache, muscle weakness, polyuria, polydipsia; no peripheral edema because of “escape” from Na retention; malignant HTN is rare
• Classically
hypokalemia
(but often normal), metabolic alkalosis, mild hypernatremia
Diagnostic studies
• 5–10% of Pts w/ HTN; ∴ screen if HTN + hypokalemia, adrenal mass or refractory HTN
• Screening:
aldo
(>15–20 ng/dL)
and
plasma aldo
:
renin ratio
(>20 if 1°) obtain 8 a.m. paired values (
off
spironolactone & eplerenone for 6 wk); Se & Sp >85%
• ACEI/ARB, diuretics, CCB can ↑ renin activity → ↓ PAC/PRA ratio and βBs may ↑ PAC/PRA ratio;∴ avoid. ɑ-blockers generally best to control HTN during dx testing.
• Confirm with
sodium suppression test
(fail to suppress aldo after sodium load) oral salt load (+ KCl) × 3 d, ✓ 24-h urine (if aldo >12 µg/d while Na >200 mEq/d)
or
2L NS over 4 h, measure aldo at end of infusion (if aldo >5 ng/dL)
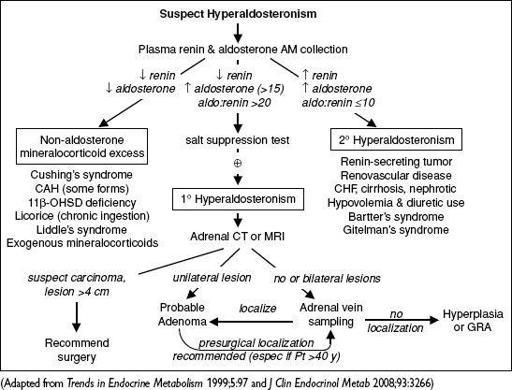
Figure 7-4
Approach to suspected hyperaldosteronism
Treatment
• Adenoma → adrenalectomy vs. medical Rx w/ spironolactone or eplerenone
• Carcinoma → adrenalectomy
• Hyperplasia → spironolactone or eplerenone; GRA → glucocorticoids ± spironolactone
ADRENAL INSUFFICIENCY
Etiologies
•
Primary
= adrenocortical disease =
Addison’s disease
autoimmune
: isolated or in assoc w/ PGA syndromes (see table on page 7-2)
infection
: TB, CMV, histoplasmosis
vascular
: hemorrhage (usually in setting of sepsis), thrombosis, HIT and trauma
metastatic disease
: (90% of adrenals must be destroyed to cause insufficiency)
deposition diseases
: hemochromatosis, amyloidosis, sarcoidosis
drugs
: ketoconazole, etomidate (even after single dose), rifampin, anticonvulsants
•
Secondary
= pituitary failure of ACTH secretion (but aldosterone
intact
b/c RAA axis) any cause of primary or secondary hypopituitarism (see “Pituitary Disorders”)
glucocorticoid therapy (can occur after ≥2 wk of “suppressive doses”; dose effect variable; <10 mg prednisone daily chronically can be suppressive)
megestrol (a progestin with some glucocorticoid activity)
Clinical manifestations
(
NEJM
1996;335:1206)
•
Primary
or
secondary
:
weakness and fatigability
(99%),
anorexia
(99%),
orthostatic hypotension
(90%), nausea (86%), vomiting (75%), hyponatremia (88%) •
Primary only
(extra s/s due to lack of aldosterone and ↑ ACTH): marked
orthostatic hypotension
(because volume-depleted), salt craving,
hyperpigmentation
(seen in creases, mucous membranes, pressure areas, nipples),
hyperkalemia
•
Secondary only
: ± other manifestations of hypopituitarism (see “Pituitary Disorders”)
Diagnostic studies
(
Annals
2003;139:194)
• Early a.m. serum cortisol: <3 µg/dL virtually diagnostic; ≥18 µg/dL rules it out (except in severe septic shock—see below) • Standard (250 µg)
cosyntropin stimulation test
(testing ability of ACTH → ↑ cortisol)
normal = 60-min post-ACTH cortisol ≥18 µg/dL
abnormal in
primary
b/c adrenal gland diseased and unable to give adequate output
abnormal in
chronic
secondary b/c adrenals atrophied and unable to respond
(very rarely, may be
normal
in
acute secondary
b/c adrenals still able to respond; early a.m. cortisol can be used rather than post-stim value in these cases)
• Other tests to evaluate HPA axis (w/ guidance by endocrinologist): insulin-induced
hypoglycemia (measure serum cortisol response); metyrapone (blocks cortisol synthesis
and therefore stimulates ACTH, measure plasma 11-deoxycortisol and urinary
17-hydroxycorticosteroid levels)
• Other lab abnormalities: hypoglycemia, eosinophilia, lymphocytosis, ± neutropenia • ACTH: ↑ in 1°, ↓ or low-normal in 2°
• Imaging studies to consider
pituitary MRI to detect anatomical abnormalities
adrenal CT: small, noncalcified adrenals in autoimmune, enlarged in metastatic disease, hemorrhage, infection or deposition (although they may be normal-appearing)
Adrenal insufficiency & critical illness
(
NEJM
2003;348:727;
JAMA
2009;301:2362)
• ↑ circulating cortisol despite ↓ ACTH due to ↓ clearance and possibly stimulation by cytokines; ∴ dx of adrenal insufficiency problematic (
NEJM
2013;368:1477) • Nonetheless, reasonable to perform ACTH stim ASAP in hypotensive Pt suspected to have absolute adrenal insuffic.
• Initiate corticosteroids early: use dexamethasone 2–4 mg IV q6h + fludrocortisone 50 µg daily prior to ACTH stim; change to hydrocortisone 50–100 mg IV q6–8h once test completed.
• Rx of
relative adrenal insufficiency
controversial (see “Sepsis”)
Treatment
•
Acute
insufficiency: volume resuscitation w/ normal saline +
hydrocortisone IV
as above •
Chronic
insufficiency
Hydrocortisone: 20–30 mg PO qd (2⁄3 a.m. 1⁄3 early p.m.) or prednisone ~5 mg PO qam
Fludrocortisone (
not
needed in 2° adrenal insufficiency): 0.05–0.1 mg PO qam
backup dexamethasone 4-mg IM prefilled syringe given to Pt for emergency situations
PHEOCHROMOCYTOMA
Clinical manifestations (five Ps)
•
Pressure
(hypertension, paroxysmal in 50%, severe & resistant to Rx, occ orthostatic)
•
Pain
(headache, chest pain)
•
Palpitations
(tachycardia, tremor, wt loss, fever)
•
Perspiration
(profuse)
•
Pallor
(vasoconstrictive spell)
• “Rule of 10”: 10% extra-adrenal (known as paraganglioma), 10% in children,
10% multiple or bilateral, 10% recur (↑ in paraganglioma), 10% malignant (↑ in
paraganglioma), 10% familial, 10% incidentaloma
• Emotional stress does not trigger paroxysms, but abdominal manipulation can trigger
catecholamine release; some reports of IV contrast causing paroxysms
• Associated with MEN2A/2B, von Hippel Lindau, neurofibromatosis type 1, familial
paraganglioma (mutations in succinate dehydrogenase gene B, C and D)
Diagnostic studies
• 24° urinary fractionated metanephrines & catechols: 90% Se, 98% Sp (
JCEM
2003;88:553). Screening test of choice if low-risk (as falsewith severe illness, renal failure, OSA, labetalol due to assay interference, TCAs, medications containing sympathomimetics).
• Plasma free metanephrines: 99% Se, 89% Sp (
JAMA
2002;287:1427). Screening test of choice if high risk, but ↑ rate of falsein low-preval. population.