Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (94 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.61Mb size Format: txt, pdf, ePub
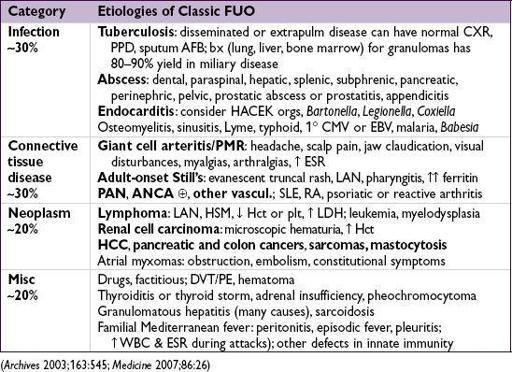
FEVER OF UNKNOWN ORIGIN (FUO)
Definition & etiologies
•
Fever
(as per above def) on >1 occasion during ≥3 wk &
no dx
despite 1 wk of evaluation • More likely to be
subtle manifestation of common disease
than an uncommon disease • In Pts with HIV: >75% causes are infectious, but
rarely due to HIV itself
•
Frequent reassessment needed
to identify focal signs and progression of disease
Workup
• Focus by H&P, incl: CBC w/ diff, lytes, BUN, Cr, LFTs, ESR, CRP, ANA, RF, cryoglobulin, LDH, CK, SPEP, 3 sets BCx (off abx), U/A, UCx, PPD or IGRA, HIV Ab ± PCR, heterophile Ab (EBV serologies if), CMV antigen, Hep serologies if LFTs abnl • Stop unnecessary meds (only 20% with a med cause have eos or rash), reassess 1–3 wk • Imaging: CXR, chest & abd CT, consider tagged WBC, gallium scan, PET, TTE, LENI • Duke’s criteria for endocarditis (qv) have good Se & Sp in Pts with FUO
• Consider temporal artery bx if ↑ ESR and age >60, particularly if other s/s • ? Bone marrow aspirate & bx (esp. if signs of marrow infiltration) or liver bx (esp. if ↑ Af): even w/o localizing s/s, yield may be up to 24% (path and culture) (
Archives
2009;169:2018) • Pursue abnormalities raised by above w/u (eg, bx, MRI, etc., for dx,
not
screening)
Treatment
• Empiric abx
not
indicated (unless Pt neutropenic) • Empiric glucocorticoids not indicated unless strong suspicion for specific rheumatologic dx • Up to 30% of cases remain undiagnosed, most spontaneously defervesce (wks to mos)
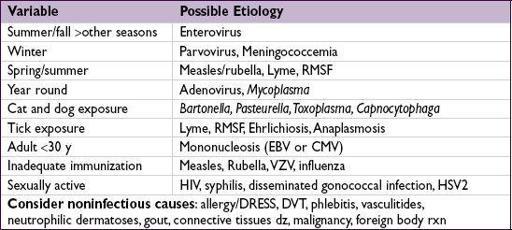
FEVER AND RASH
Approach to diagnostic workup
•
Meningococcemia, IE, RMSF, sepsis, toxic shock require immediate dx & Rx
• Workup: CBC w/ diff, lytes, BUN/Cr, LFTs, LDH, CK, U/A, HIV Ab ± PCR, BCx (off abx)
• To narrow Ddx: characterize time course of rash, progression & morphology (ie, vesicular, maculopapular, pustular, purpuric, ulcerative) •
Erythema multiforme
: symmetric “target” lesions often of palms, soles, & mucous memb
Infxn etiol: HSV 1/2,
Mycoplasma
, syphilis, tick borne diseases,
etc.
Non-infxn etiol: meds (eg, NSAIDs, sulfa), malignancy, autoimmune & rheum disease
•
Erythema nodosum
: tender erythematous or violaceous nodules usually symmetric on LE
Infxn etiol: Strep, TB, EBV,
Bartonella
, HBV, psittacosis, fungal,
L. venereum
,
etc.
Non-infxn etiol: sarcoidosis, IBD, Behçet’s, other rheum, pregnancy/OCP use
• Pursue specific dx based on exposure hx & exam, including serologies, viral swab PCR, antigen tests and possibly skin biopsy ± exam of vesicular or bullae fluid if present • Etiologies more broad in immunosupp. Pts, and dx approach usually more extensive; higher risk of critical illness due to disseminated or rapidly progressive infxns
Treatment
• Empiric abx are
not
indicated (unless Pt neutropenic or critically ill)
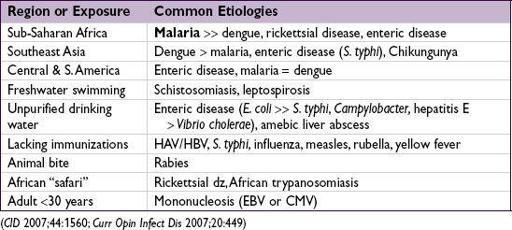
FEVER IN A RETURNED TRAVELER
Definition & etiologies
• Febrile illness after recent travel outside of U.S./Canada; Ddx is extensive:
• Pts visiting friends and relatives abroad are most likely to contract illness during travel • Emerging pathogens: Influenza occurs year round in the tropics. Chikungunya and dengue w/ ↑ areas of transmission, hemorrhagic fevers primarily in Central Africa.
• Consider domestic infxns, STIs, & non-infxn causes. Enteric parasites rarely cause fever.
Select clinical manifestations
•
Malaria
: nonspecific symptoms including diarrhea, myalgias, cough, altered mental status •
Dengue
: nonspecific symptoms including headache, severe myalgias, rash/petechiae •
Typhoid
: constipation, abdominal pain, possible rash, relative bradycardia •
Rickettsial disease
: headache, myalgias, lymphadenopathy, possible rash/eschar
Workup
• Routine testing: CBC w/ diff, lytes, LFTs, BCx, UA, rapid malaria test
•
Fever in a traveler from a malaria zone is malaria until proven otherwise; consider hospitalization and empiric Rx.
Onesmear does
not
r/o malaria.
• Other tests based on s/s, labs, exposure, incubation period, geography and seasonality. O&P exam, CXR, blood smears for filaria/Babesiosis/
Borrelia
, serologies, STI & HIV, PPD or IGRA, bone marrow aspirate, bx of lymph nodes or skin lesions, CSF studies.
NOTES
PITUITARY DISORDERS
HYPOPITUITARY SYNDROMES
Panhypopituitarism
• Etiologies
Primary
: surgery, radiation, tumors (primary or metastatic), infection, infiltration (sarcoid, hemochromatosis), autoimmune, ischemia (including Sheehan’s syndrome caused by pituitary infarction intrapartum), carotid aneurysms, cavernous sinus thrombosis, trauma
Secondary
(hypothalamic dysfunction or stalk interruption): tumors (including craniopharyngioma), infection, infiltration, radiation, surgery, trauma
• Clinical manifestations
Hormonal
: acute → weakness, easy fatigability, hypotension, polyuria and polydipsia; chronic → bradycardia, sexual dysfxn, loss of axillary & pubic hair, wt loss, amenorrhea
Mass effect
: headache, visual field Δs, cranial nerve palsies, galactorrhea
Apoplexy
(pituitary hemorrhage or infarction, usually w/ underlying pituitary adenoma): sudden headache, N/V, visual field Δs, cranial nerve palsies, meningismus, Δ MS, hypoglycemia, hypotension
• Diagnostic studies
Hormonal studies
chronic:
↓ target gland hormone + ↓ or normal trophic pituitary hormone
acute:
target gland hormonal studies may be
normal partial hypopituitarism is more common than panhypopituitarism
Pituitary MRI
• Treatment
Replace deficient target gland hormones
Most important deficiencies to recognize and treat in inPts are
adrenal insufficiency
and
hypothyroidism;
if both present, treat with glucocorticoids first, then replace thyroid hormone so as not to precipitate adrenal crisis
↓ ACTH
• Adrenal insufficiency similar to 1° (see “Adrenal Disorders”)
except:
no salt cravings or hypokalemia (b/c aldo preserved)
no hyperpigmentation (b/c ACTH/MSH is not ↑)
↓ TSH
• Central hypothyroidism similar to 1° (see “Thyroid Disorders”)
except
absence of goiter • Dx with free T
4
in addition to TSH, as TSH may be low or
inappropriately normal
↓ PRL
• Inability to lactate
↓ GH
• ↑ chronic risk for osteoporosis, fatigue, weight gain • Dx with failure to ↑ GH w/ appropriate stimulus (eg, insulin tolerance test, glucagon stimulation) • GH replacement in adults controversial (
Annals
2003;35:419)
↓ FSH & LH
• Clinical manifestations: ↓ libido, impotence, oligomenorrhea or amenorrhea, infertility • Physical exam: ↓ testicular size; loss of axillary, pubic and body hair • Dx with: ↓ a.m. testosterone or estradiol (also assess SHBG, esp. in obese) and ↓ or normal FSH/LH (all levels ↓ in acute illness, ∴ do not measure in hospitalized Pts) • Treatment: testosterone or estrogen replacement
vs
. correction of the underlying cause
↓ ADH
(hypothalamic or stalk disease): diabetes insipidus
• Typically from mass lesion extrinsic to sella; pituitary tumor doesn’t typically present w/ DI • Clinical manifestations:
severe
polyuria,
mild
hypernatremia (
severe
if ↓ access to H
2
O) • Diagnostic studies: see “Sodium and Water Homeostasis”
Other books
The Legacy by Malley, Gemma
Pure & Sinful (Pure Souls) by McRae, Killian
Nash's Niche (Behind Closed Doors) by McAllan, Raven
Colmillos Plateados by Carl Bowen
TheDungeon by Velvet
Six Feet Over It by Jennifer Longo
Past Sins by Debra Webb
Full Tilt by Janet Evanovich
The Immortal Game by Miner, Mike