Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (99 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
3.12Mb size Format: txt, pdf, ePub
• Adrenal CT or MRI; consider MIBG scintigraphy if CT/MRI, PET can be used to
localize nonadrenal mass, but usually easy to find
• Consider genetic testing in appropriate circumstances (bilateral, young Pt,FHx, extra-adrenal)
Treatment
• ɑ-blockade first (usually phenoxybenzamine) ± β-blockade (often propranolol) → surgery
• Preoperative volume expansion is critical due to possible hypotension after tumor excision
ADRENAL INCIDENTALOMAS
Epidemiology
• 4% of Pts undergoing abdominal CT scan have incidentally discovered adrenal mass; prevalence ↑ with age
Differential diagnosis
•
Nonfunctioning mass
: adenoma, cysts, abscesses, granuloma, hemorrhage, lipoma,
myelolipoma, primary or metastatic malignancy
•
Functioning mass
: pheochromocytoma, adenoma (cortisol, aldosterone, sex hormones), nonclassical CAH, other endocrine tumor, carcinoma •
Nonadrenal mass
: renal, pancreatic, gastric, artifact
Workup
(
NEJM
2007;356:601;
JCEM
2010;95:4106)
•
Rule out subclinical Cushing’s syndrome
in all Pts
using 1 mg overnight DST (Sp 91%). Abnormal results require confirmatory testing.
•
Rule out hyperaldosteronism
if hypertensive
w/ plasma aldo & renin (see above) •
Rule out pheochromocytoma
in ALL Pts
(b/c of morbidity unRx’d pheo) using 24-h urine fractionated metanephrines and catecholamines or plasma free metanephrines • Rule out metastatic cancer and infection by history or CT-guided biopsy if suspicious (in Pts w/ h/o cancer, ~50% of adrenal incidentalomas are malignant) • CT and MRI characteristics may suggest adenoma vs. carcinoma
Benign features:
size <4 cm; smooth margins, homogenous and hypodense appearance; unenhanced CT <10 Hounsfield units or CT contrast-medium washout >50% at 10 min. Can follow such incidentalomas w/ periodic scans.
Suspicious features:
size >4 cm or ↑ size on repeat scan; irregular margins, heterogeneous, dense or vascular appearance; h/o malignancy or young age (incidentaloma less common). Such incidentalomas warrant resection or repeat scan at short interval.
CALCIUM DISORDERS
Pitfalls in measuring calcium
• Physiologically active Ca is free or ionized (ICa). Serum Ca reflects total calcium (bound + unbound) and ∴ influenced by albumin (main Ca-binding protein).
• Corrected Ca (mg/dL) = measured Ca (mg/dL) + {0.8 × [4 − albumin (g/dL)]}
• Alkalosis will cause more Ca to be bound to albumin (∴ total Ca may be normal but ↓ ICa) • Best to measure
ionized Ca directly
(but accuracy is lab dependent)
HYPERCALCEMIA
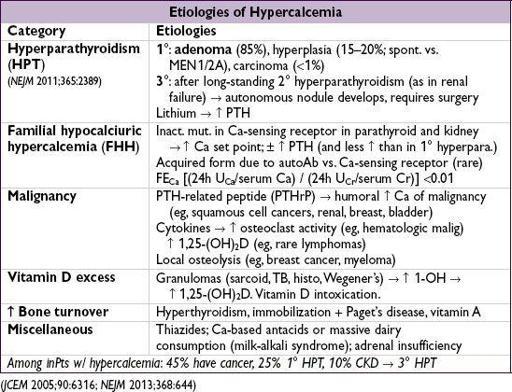
Clinical manifestations
(“bones, stones, abdominal groans and psychic moans”)
•
Hypercalcemic crisis
(usually when Ca >13–15): polyuria, dehydration, ΔMS
Ca toxic to renal tubules → blocks ADH activity, causes vasoconstriction and ↓ GFR → polyuria but Ca reabsorption → ↑ serum Ca → ↑ nephrotoxicity and CNS sx
• Osteopenia, fractures and osteitis fibrosa cystica (latter seen in severe hyperpara. only →
↑ osteoclast activity → cysts, fibrous nodules, salt & pepper appearance on X-ray)
• Nephrolithiasis, nephrocalcinosis, nephrogenic DI
• Abdominal pain, anorexia, nausea, vomiting, constipation, pancreatitis, PUD
• Fatigue, weakness, depression, confusion, coma, ↓ DTRs, short QT interval • 1° HPT: 80% asx, 20% nephrolithiasis, osteoporosis,
etc.
•
Calciphylaxis
(calcific uremic arteriopathy): calcification of media of small-to med-sized blood vessels of dermis & SC fat → ischemia and skin necrosis (
NEJM
2007;356:1049).
Associated w/ uremia, ↑ PTH, ↑ Ca, ↑ PO
4
and ↑ (Ca × PO
4
) product. Dx by biopsy.
Rx: aggressive wound care, keep Ca & PO
4
nl (goal <55), avoid vitamin Δ & Ca suppl. IV Na thiosulfate, cinacalcet, & parathyroidectomy controversial.
Overall portends a poor prognosis
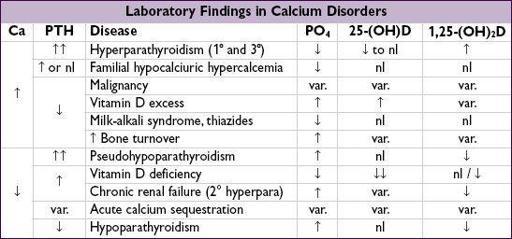
Diagnostic studies
• Hyperparathyroidism and malignancy account for 90% of cases of hypercalcemia
hyperparathyroidism more likely if asx or chronic hypercalcemia
malignancy more likely if acute or sx; malignancy usually overt or becomes so in mos
• Ca, alb, ICa, PTH (may be inappropriately normal in 1° HPT & FHH), PO
4
;
↑ or high nl PTH: 24-h U
Ca
>200 mg → HPT; 24-h U
Ca
<100 mg & FE
Ca
<0.01 → FHH
↓ PTH: ✓ PTHrP, AΦ, & search for malig (eg, CT, mammogram, SPEP/UPEP) and ✓ vit D: ↑ 25-(OH)D → meds; ↑ 1,25-(OH)
2
D → granuloma (✓ CXR, ACE, r/o lymph)
Treatment of asymptomatic 1° HPT
(JCEM 2009;94:335)
• Surgery if: age <50 y; serum Ca >1 mg/dL >ULN; CrCl <60 mL/min, DEXA T score <-2.5
• If surgery declined/deferred, can Rx with bisphosphonates (↑ BMD but do not ↓ Ca & PTH) or cinacalcet (↓ Ca & PTH but may not ↑ BMD) • If not yet candidate for surgery: ✓ serum Ca & Cr annually and BMD q1–2y
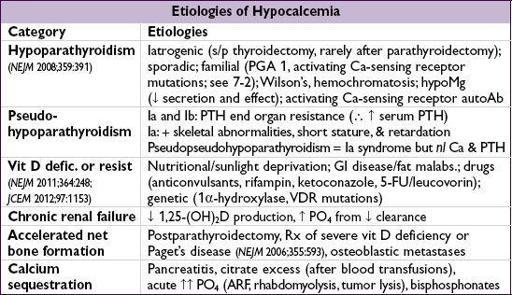
HYPOCALCEMIA
Clinical manifestations
•
Neuromuscular irritability
: perioral paresthesias, cramps,Chvostek’s
(tapping facial nerve → contraction of facial muscles),Trousseau’s
(inflation of BP cuff → carpal spasm), laryngospasm; irritability, depression, psychosis, ↑ ICP, seizures, ↑ QT
Other books
Strum Your Heart Out by Crystal Kaswell
Cherished by Barbara Abercrombie
Blood On the Wall by Jim Eldridge
My Billionaire Stepbrother by Sterling, Jillian
Dos días de mayo by Jordi Sierra i Fabra
The Beet Fields by Gary Paulsen
Billionaire Romance: Flame by Stephanie Graham
Revelations (Bloodline Series) by Kendal, Lindsay Anne
Centyr Dominance by Michael G. Manning
Breathe for Me by Rhonda Helms